Annals
of the M.B.C. - vol. 1° - n° 2 - September 1988
PRELIMINARY CONSIDERATIONS ON HAEMOCOAGULATIVE PROBLEMS
FOLLOWING SERIOUS BURNS
Argano
S.P.A., Spilotros G., Cardinale G., Pitres V., Bologna R, D'Arpa N.
Servizio di Ematologia USL 58 - Palermo
Centro Ustioni USL 58 - Palermo, Italia
SUMMARY .
Haemocoagulative complications after serious bums are a constant feature, and very often
represent a considerable clinical problem. Our preliminary observations of 15 patients
sent to us by the U.S.L. 58 Bums Centre indicate that the burn lesion gives rise to a
series of haematological modifications, beginning with a phase of hypercoagulability
immediately after the burn injury, followed by activation of fibrinolysis and finally a
coagulative rebound. In some cases the appearance of shock, sepsis or the liberation into
the bloodstream of tissue activators can precipitate an acute condition of intravascular
coagulation, whose diagnostic predictability using the tests currently available for
haemocoagulative studies is in any case uncertain, and possibly even controversial.
Among traditional tests an important place is occupied by the study of thromboeytosis and
platelet function. Our efYorts are therefore now directed at the search for valid
parameters which through simple and straightforward investigations will make it possible
to make a more precise assessment of haemostatic disorders, with a view to preventing any
subsequent more serious haemocoagulative imbalances. We therefore believe that the
inclusion of tests for Protein C evaluation, 17PA and antifibrinolysins in standard
laboratory protocol, together with the study of the bone marrow and RES clearance, when
possible, will provide us with more useful and more complete data for better clinical
surveillance and a more rational therapy.
Introduction
The
modification of routine haemocoagulative parameters in burn pathology is a fairly common
finding.
As a result of marked imbalances in haemostatic equilibrium, there may sometimes be cases
of severe haemorrhage which represent a grave clinical problem, possibly even leading to
the death of the burn victim.
The subject of this paper is the monitoring of the common haemocoagulative parameters and
the interpretation of their modifications in the course of burn pathology.
Materials and methods
We studied 15
patients with burned BSA over 30%, aged between é and é5 years. All of these had 2nd or
3rd degree burns.
Blood samples were taken immediately upon admission, then every other day during the first
2 weeks and then weekly until the patient was discharged from the intensive care unit.
The blood was removed
from the artery or vein and was placed in a test tube with K3 EDTA (1 mg/ml) for haemochromocytometric study and
platelet count, and in a test tube with Na Citrate 0.1 M (1:10) for prothrombin time (PT),
activated partial thromboplastin time (aPTT) and fibrinogen. The Quick method (1) was used
for PT, bovine cephalin and ellagic acid for aPTT, the Clauss method (2) for fibrinogen,
and the latex method (3) for fibrinogen/fibrin degradation products (FDP). All
haemocoagulative findings were obtained with the aid of an MLA Electra 750 semiautomatic
coagulometer.
Results
Of the 15
patients studied, é died, 4 as a result of infective complications and 2 of kidney
failure. Among the 9 survivors PT and aPTT remained within normal limits 48-72 hours after
the burn lesion, then increased gradually to reach a peak between the 9th and 13th day.
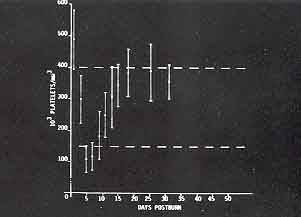
These values returned to normal in 2-3 weeks (Figs. 1, 2). Fibrinogen concentration was
low in the first 24 hours, then increased progressively to a peak on day 9, returning to
normal in the next 3 weeks (Fig. 3). The FDP were normal in the first 3-5 days after the
burn and then remained at high values in the following 4 weeks, peaking between days 9 and
12 (Fig. 4). Initial thrombocytosis was followed by a rapid drop in the platelet count,
which reached its lowest point on day 5, after which there was a gradual return to
normality, or in some cases slightly higher than normal values, in the next 3-4 weeks.
In the 4 patients who died as a result of infective complications, we observed a
progressive deterioration of the haemocoagulative parameters, especially with regard to
thrombocytosis. These modifications of haemostatic equilibrium seemed to be connected with
the onset of sepsis. In one case there was disseminated intravascular coagulopathy.
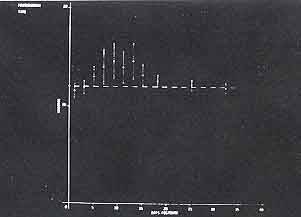 Fig. 1 |
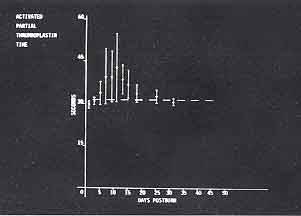 Fig. 2 |
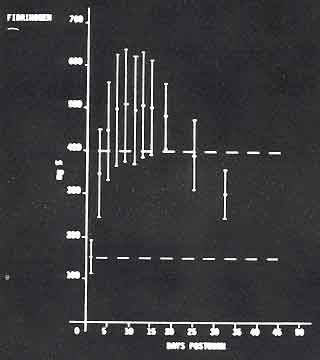 Fig. 3 |
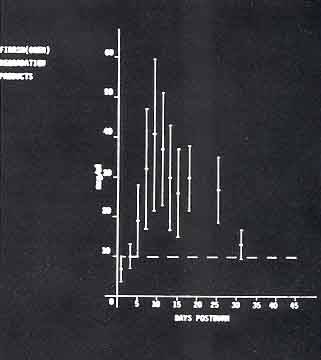 Fig. 4 |
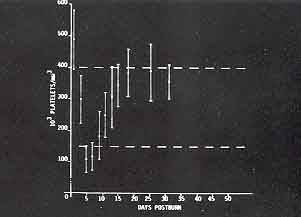 Fig. 5 |
|
|
Discussion
The findings show
that the haemocoagulative condition of the burn patients varied in relation to the
modification of their physiopathological conditions.
In the first phase, in the hours immediately following the bum lesion, we observed a
hypercoagulative modification due mainly to the massive liberation of thromboplastin
tissue factors and to haemoconcentration.
During this phase we recorded thrombocytosis, normal MP, PT and aPTT values and
hypofibrinogenaemia, the latter being due to increased consumption in the burned areas and
to the sequestrum in the interstitial space.
This was followed by a phase of hypocoagulability beginning about the 2nd to the 5th day,
during which period we recorded a lengthening of PT and aPTT, in relation to excessive
peripheral utilization and to reduced synthesis of the coagulation factors; we also
observed a drop in thrombocytosis, due to peripheral consumption and to a non regenerative
bone marrow condition (4); hyperfibrinogenaemia, caused by increased synthesis and a
reduction of losses (5) and also by pyrogens and other bacterial extracts, their efflect
being mediated by the leukoeytes (é); and an increase in the FDP as a result of
degradation of fibrin and fibrinogen at intravascular and interstitial level in the bum
sites (5).
FDP concrentration remained above normal for most of the observation period, and we
observed haemorrhagic manifestations in only one case; this parameter is thus only a rough
guide to identifying the various haemocoagulative modifications following severe bums; FDP
concentration is of greater significance in complicated cases of sepsis and shock, when
accompanied by serious impairment of the other haemocoagulative parameters, particularly
thrombocytopenia; however, even in this case, the finding is of poor predictive value as
it comes too late.
This phase of fibrinolytic activation and of consumption lasted for variable periods,
subsequently developing towards a return to conditions of normal coagulability, or to a
new hypercoagulative phase for which a number of trigger mechanisms are responsible, such
as endotoxins, circulating immunocomplexes, acidosis, hypoxia and a relatively inefficient
RES clearance. Persistent thrombocytopenia is a negative prognostic sign, as the
platelets, due to their rapid turnover, are an important warning signal of the degree of
medullary inhibition and of the peripheral procoagulative stimulus (7).
Some other parameters, such as the concentrations of ATIll, FPA, Beta TBG, PF4, Protein C,
D Dimers, t-PA and PK, have been introduced comparatively recently into laboratory
practice. They help to cast light on the various phenomena that occur in haemostasis,
regarding both coagulation and fibrinolysis; any modification of these parameters could be
a warning signal of a condition which from an initial subclinical level might evolve
towards a more serious condition like DIC.
The literature is beginning to describe the first limited data suggesting that some of
these parameters ' in particular ATIII and PIC, might have some predictive value in
the case of burn lesions (8).
The purpose of our ongoing study is to identify, if possible, among the data that will
accumulate from a routine use of these tests a correlation with the survival of burn
patients.
Also, whenever it is possible to perform tests on patients in a condition of general
anaesthesia, the haemotopoietic condition will be examined by means of multiple needle
aspirations and needle biopsies of bone marrow, the efficiency of RES clearance being
checked at the same time.
We hope that these procedures will provide us with information on the basis of which it
will be possible to draw up a protocol of clinical and laboratory control enabling us to
formulate predictions regarding haemocoagulative conditions, i.e. to foresee the turning
point towards conditions of hypercoagulation when there is still time to initiate correct
therapy.
RÉSUMÉ. Les
altérations hémo-coagulatrices au cours d'une grave brûlure sont constantes et
représentent souvent un probl&me clinique considérable.
Nos observations préliminaires sur 15 patients que le Centre des Brûlés USL 58 nous a
envoyés conduisent a reconnaitre dans la brûlure une dynamique des modifications
hématologiques ou a une phase d'hypercoagulation, immédiatement aprés I'accident, suit
une activation de la production de fibrine et enfin un "rebound" coagulateur. En
certains cas, un choc, une septicémie ou la libération d'activateurs du tissu peuvent
accélérer une condition aigiie de coagulation intra-vasculaire, dont le diagnostic n'est
pas aisé a prévoir avec les tests dont on dispose actuellement pour 1'étude
hémo-coagulatrice.
Parmi les tests traditionnels, 1'étude du nombre des plaquettes et de la foriction
plaquettaire occupe une place importante. Par conséquent nos efforts se tournent
actuellement vers la recherche de paramétres valables, à travers des enquétes
d'exécution simple et rapide, de maniére à consentir une estimation plus précise des
troubles hémostatiques pour prévoir d'éventuels déséquilibres graves en matiére
d'hémo-coagulation. Nous retenons en outre qu'il faut introduire des tests pour évaluer
la protéine C, les FPA, et les antiplasmines dans le contréle de laboratoire,
parallélement à l'étude de la moelle osseuse et de la clearance du SRE, chaque fois que
ce sera possible, pour nous fournir des indications plus complétes et utiles pour une
surveillance clinique meilleure et une thérapic plus rationnelle.
BIBLIOGRAPHY
- Quick A.J.: Hemorrhagic diseases
and thrombosis. 2nd ed. Lea and Febiger, Philadelphia, 1966.
- Clauss H.: Acta Haematol 17: 237,
1957,
- Garvey M.B.: J. Clin. Pathol. 25:
680, 1972.
- Eurenius K.: J. Lab. Clin. Med.
79: 247, 1972.
- Baxter C.R.: Surgery 77: 86, 1975.
- Rapaport S.I.: Thromb. and
Hemostas. 35: 692, 1976.
- Eurenius K.: Proc. Soc. Exp. Biol.
and Med. 147: 878, 1974.
- Brown J.M.: Thromb. Res. Suppl. VI
p. 153, 1986.
|