Annals
of the M.B.C. - vol. 1° - n° 2 - September 1988
PREVENTION AND THERAPY OF ACUTE RENAL FAILURE IN
SEVERELY BURNED PATIENTS
Manni C.
Istituto di
Anestesiologia e Rianimazione Universita Cattolica del S. Cuore - Roma, Italia
SUMMARY.
In burn casualties, renal function is severely affected. In the treatment of these
cases prevention of renal failure is fundamental in preventing complications and death.
Maintenance of the efficiency of renal function is based on water and salts
administration, control of cardiac, vascular and respiratory functions and prevention of
infections.
In the treatment of impending or actual renal failure the following points must be
considered:
- Evaluation of kidney function by assessing the variations of different parameters of
renal performance.
- Conduct of proper therapeutic intervention to substitute the efFects of renal failure
(dialysis), to minimize their damage to the total organism, and to facilitate clinical
recovery (nutrition).
In
patients with severe and extensive burns, the renal function can rapidly be endangered by
shock, by hypovolaemia, by the loss of the trauma plasma proteins, by hydroelectrolyte
imbalances and by the neuroendocrine response to stress.
Taking into consideration the high mortality rate caused by acute renal failure, every
etTort must be made to spot the first signs of functional failure which always precede
anatomical damage. The aim is to adopt at this stage all the efficacious prophylactic
measures available.
To reach this primary objective it is indispensable to adopt a system of multi-parametric
monitoring which uses a large range of date, some measured directly, others calculated.
When we decided to begin this type of monitoring we found there were difficulties linked
to the value and the meaning to be attributed to the numerous parameters proposed by
different authors; we thus had to make a preliminary selection.
Besides having to operate in emergency we had to overcome the difficulties linked to the
time needed for the calculation of certain values. Fortunately, the use of the computer,
with "ad hoc" programs, now enables us to carry out this type of
multi-parametric evaluation in real time.
These programs, besides indicating the degree. of alteration of the function, also
facilitate the differential diagnosis among the various possible causes of renal damage.
A preliminary analysis of this problem was necessary in order to realize a program of
diagnostic and therapeutic aid. This could be schematized by the algorithms relative to
the typical situations which are characteristic of certain types of renal failure:
oliguria and anuria.
The appearance of anuria, once the presence of postrenal causes has been excluded, demands
the prompt adoption of specific therapeutic measures. It must be kept in mind, in this
case, that when there is no urine it is impossible to carry out a whole series of
fundamental analyses. It is therefore necessary to base our handling of the case on
haemodynamic and serum parameters as well as on the modifications we observe in response
to those therapeutic measures which we gradually adopt. If hypovolaemia is present
(Central Venous Pressure (CVP) less than 10 cm H 20 or
Pulmonary Capillary Wedge Pressure (PCWP) less than 18 mmHg) it can be corrected by the
infusion of a suitable quantity of colloids and crystalloids. At a later stage an attempt
can be made to restore diuresis by means of the infusion of mannitol. At the same time the
administration of 3-5 gamma/Kg/min of doparnine, which increases the renal blood flow, can
be begun without -causing other unwanted haemodynamic effects.
If the volaemia is normal or increased (CPV higher than 10 cm H 2 0 or PCWP higher than 18 mmHg) the
infusion of dopamine can be begun immediately with the same dosage, and that of fusemide
with a high dosage (Img/Kg/hour). In normovolaemic and anuric patients, the administration
of mannitol, even in small doses, should be avoided because of the risk of causing
congestion or pulmonary oedema. The lack of response to these interventions is a signal to
begin dialysis therapy.
In the presence of oliguria our behaviour will be different from that in the case of
anuria since in these patients we are able to distinguish directly functional failures
from organic ones.
In this sense, as we have already stated, the computer can help us especially in
determining the parameters which will tell us the type of failure which is present.
The difterential diagnosis (Fig. 1) derives from the relative modifications of the
following parameters: specific weight of the urine; urinary osmolality; the clearance of
free water; the concentration of sodium in the urine; the excretion fraction of sodium (Na
E17); the index of renal failure; the urinary serum ratios of creatinine and ureic
nitrogen.
Oliguria |
| |
Renal
failure |
| Parameters |
Prerenal |
A.T.N. |
| Urinary specific weight |
> 1020 |
< 1012 |
| UOsm (mOsm/Kg/H2O) |
> 500 |
< 350 |
| OUT. Osm (mOsm/24 h) |
> 600 |
< 400 |
| U Osm/S Osm |
> 1.2 |
< 1.0 |
| CH2O (ml/h) |
<- 25 |
>- 15 |
| U Na (mEq/1) |
< 20 |
> 40 |
| Na EF |
< 1 |
> 1 |
| R.F.I. |
< 1 |
> 1 |
| U/S creatinine |
> 40 |
< 20 |
| U/S urea nitrogen |
> 8 |
< 3 |
Fig.
1 |
|
It is important to stress that these parameters, if
taken individually, have a varying degree of reliability.
Recent evaluations have enabled us to establish thar the most reliable are the excretion
fraction of sodium and the index of renal failure.
However, the evaluation of all the parameters selected enables us to make a surer
judgement for the differential diagnosis between functional and organic forms.
Finally, we can take this opportunity to recall that ARF is not always associated with
oligoanuria: in fact, forms in which diuresis is maintained are very frequent. In high
risk patients it is therefore indispensable always to monitor the renal function even in
the absence of oliguria.
With this in mind, we would like to give an example of the use of computerized monitoring
adopted by us.
In the first place, the data for the identification of the patient and the values of the
parameters measured are fed into the computer (Fig. 2). Then the computer proceeds to the
calculation of the derived parameters (Fig. 3).
Hydroelectrolytic
balance and renal function
Measure parameter |
| |
Urinary vol. |
(ml) |
835 |
| Time |
(Hr) |
8 |
| Urine |
Sodium |
(mEq/l) |
51 |
| Potassium |
(mEq/l) |
58 |
| Urea |
(g/l) |
9.31 |
| Creatinine |
(g/l) |
0.49 |
| Osmolality |
(mOsm/Kg) |
754 |
| Serum |
Glucose |
(mg/dl) |
165 |
| Sodium |
(mEq/l) |
141 |
| Potassium |
(mEq/l) |
5.3 |
| Chloride |
(mEq/l) |
103 |
| BUN |
(mg/dl) |
16 |
| Creatinine |
(mg/dl) |
0.9 |
| Osmolality |
(mOsm/Kg) |
278 |
|
Hydroelectrolytic
balance and renal function
Calculated parameters |
| Std. creat. cl. |
(ml/min) |
98.78 |
| Std. urea cl. |
(ml/min) |
49.24 |
| Std. osm. clear. |
(ml/h) |
283.09 |
| Free water clear. |
(ml/h) |
- 178.7 |
| Osm. out./24 Hr |
(mOsm) |
1888.7 |
| U. Osm./s. osm. |
|
2.71 |
| U. Na/U.K |
|
0.879 |
| U. creat./s. creat. |
|
54.44 |
| U. urea/s. urea |
|
27.14 |
| BUN/s. creat. |
|
17.78 |
| Na EF |
(%) |
0.664 |
| Renal fail. index |
(%) |
0.937 |
|
| Fig. 2 |
Fig. 3 |
|
From an
overall evaluation of the tables supplied by the computer program, the state of renal
functionality and of the specific hydro-electrolyte imbalances, which demand immediate
correction, can be established with precision.
Once the diagnosis of "acute tubulonecrosis" has been made, it is clearly
indispensable to begin immediately a therapy whose foundations are haemodialysis and
clinical nutrition.
Much experience has in fact well documented the advantages of specific diets which improve
the general conditions of the patient, prevent certain complications caused by uraemic
intoxication and delay the beginning of dialysis or lessen its frequency.
Unfortunately, the appearance of anorexia, omiting, gastro-intestinal failure and
respiratory failure often hinder adequate alimentation per os.
In this case, if parenteral nutrition is not promptly adopted, the lack of food intake and
increased catabolism rapidly bring about a state of serious malnutrition whose effects
have a significant influence on the evolution of the pathology.
Unfortunately, in these patients, a correct and efficacious parenteral nutrition meets
numerous difficulties. For the most part, these are linked to the metabolic alterations
which constantly occur in the course of renal failure. These metabolic alterations have
not yet been sufficiently clarified, but they are closely correlated, complex and
dynamically evolving; and they effect the carbohydrate, lipid and protein metabolism.
If one wants to assign a therapeutic role to nutrition, a sequential analysis of the
evolutionary phases of the clinical situation is indispensable so that what should be
done, and how and when, can be accurately programmed. The complete response to these
questions does not in fact exist since precise and definitive criteria are not yet
available. There do exist, however, principles which it is necessary to uphold, if only to
respect the oldest, but still valid, commandment of medicine: "primum non
nocere": first do no harm through actions or omissions.
For this reason, it is necessary to stress the need to evaluate attentively the single
specific problems which can modify our nutritional strategy day by day. In particular we
note sodium, potassium and water retention, the onset of metabolic acidosis, the high
levels of ureic nitrogen, the increased demand for the essential aminoacids, the
heightened susceptibility to infections, frequent plurisysternic failure and the
altered utilization of the energy and plastic substrata.
Taking into consideration that these conditions are often present at the same time and are
reciprocally damaging, one can form an idea of the operative difficulties one can meet in
the indispensable application of an appropriate and safe parenteral nutrition.
It is possible to supply some indications on the quantitative and qualificative choices of
the energyplastic supply which enable us to improve the nutritional state of these
patients without causing a metabolic overload of the complications they carry with them.
With regard to the calorie supply, the choice of the energy substratum is fundamental for
the realization of an efficacious and at the same time safe nutritional programme.
There are two possible alternatives: either to use glucose as the only calorie source (the
Glucose System) or to use both glucose and lipids (the GlucoseLipids System). Both of
these solutions have advantages and disadvantages and specific indications.
The Glucose System enables the physician to infuse a high quantity of calories in small
volumes by using solutions of 50-70%. It is suggested that, in the case of all those
patients with excess water, this be corrected first with appropriate dialysis therapy.
A counterindication for the use of glucose as the only calorie source is the
well-documented intolerance associated with the uraemic syndrome, with a tendency to
hyperglycaemia and the reduction of the hypoglycaemizing and anabolizing action of
insulin.
Infusion with glucose only can also be associated with the inhibition of lipogenesis, an
increase in the oxydization of the glucose and of the glycogen deposit, an increase of the
catecholamines, increased consumption of O2 and increased production of CO2.
The use of glucose only is not advisable in the presence of respiratory failure and in the
case of patients in mechanical ventilation.
On the other hand, the combined Glucose-Lipids System has numerous advantages: less
metabolic overload compared to the infusion of a single substratum, the supply of the
essential fatty acids, the diminished frequency of hyperglycaemia and hepatic steatosis
and a reduced production of CO2 and consumption of O2.
With regard to the nitrogen supply, it is indispensable that it should be sufficient to
supply the needs of the organism. For many years, in order to reduce the accumulation of
the products of protein degradation which are potentially toxic and to favour the
utilization of the urea as a source of nitrogen for the organism, hypoprotein-hypercalorie
diets have been adopted. In fact, in the majority of cases, this method hindered the
control of the toxic symptomatology and almost always worsened the condition of
malnutrition.
Given the present state of knowledge, the hypothesis seems to emerge that with a timely
and qualitative choice of alimentation and with appropriate dialysis it is possible to
increase the quantity of the protein supply with the result of a rapid restoration and
maintenance of a good nutritional equilibrium. The reaching of this objective is
facilitated by the moderate use of proteins with a high biological value. The ratio
essential aminoacids/total nitrogen must therefore always be greater than 3 to 1.
From what has been said (Fig. 4) it is possible to compile four different parenteral
nutrition programmes.
Acute
renal failure
Parenteral nutrition |
|
Glucose
system |
Glucose - Lipids system |
| Calories
(Keal/Kg/dic) |
30 |
30 |
40 |
50 |
| Aminoacids
(g/Kg/dic) |
0.35 |
0.5 |
1 |
1.5 |
| Calories/N ratio |
520:1 |
375:1 |
250:1 |
205:1 |
| Glucose (g/Kg/die) |
8 |
4.6 |
6 |
8 |
| Lipids (g/Kg/die) |
- |
1.4 |
1.4 |
2.1 |
| EAA (g/Kg/die) |
0.35 |
0.35 |
0.6 |
0.8 |
| EAA/Total N ratio |
- |
4.4 |
3.75 |
3.3 |
Type |
1 |
2 |
3 |
4 |
|
|
|
The data are
obviously indicative and must be considered exclusively as reference data. Personalization
of the nutritional therapy, as far as possible, is always mandatory.
Programme 1 envisages the infusion of glucose as the single source of calories plus
essential aminoacids, the latter being the only source of nitrogen. It is indicated for
patients with a water overload, electrolyte imbalances, metabolic acidosis and high values
of ureic serum nitrogen, to allow time for dialysis therapy to correct the above-mentioned
alterations.
This programme can never be continued for a long period of time.
Programme 2 (Isocaloric-Hypoprotein) is indicated during those days when dialysis therapy
is not carried out and in the period of resumption of renal function after acute renal
failure until creatinine clearance rises above 20 ml/min.
Programmes 3 and 4 are indicated for patients in dialysis therapy. Only these are able to
satisfy the high energy-plastic needs of patients with extensive burn. They should be
adopted as soon as possible.
In conclusion we can safely affirm that we possess today sufficient diagnostic and
therapeutic means to treat with good prospects of success acute renal failure even in
patients suffering from severe burns and/or multiple parenchymal failures.
- - Computerized multi-parametric
monitoring facilitates early diagnosis.
- - Aggressive dialysis technique
permits a valid conrol of endotoxicosis.
- - Parenteral nutrition favours the
maintenance of a normal nutritional state and avoids the complications of malnutrition.
Respect for these three fundamental procedures in the treatment of
acute renal failure in critical patients has enabled us (Fig. 5) to reduce progressively
and significantly the mortality rate which is linked to these complications. From 1971 to
1986, it has progressively fallen from 79% to 42% in the cases we treated.
Policlinico Universitario "A.
Gemelli"
Intensive Care UnitAcute Renal Failure
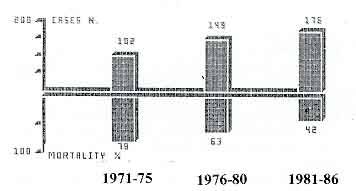
|
Fig. 5 |
|
RÉSUMÉ.
11 est trés fréquent que la fonction rénale se trouve affectée chez les
victims de brûlures graves. Dans le traitement de ces cas la prévention d'une crise
rénale est fondamentale pour éiter les complications et la mort.
Pour maintenir en pleine efficacité la fenction rénale, it taut administrer de I'eau et
des sets, contréIer la fonction cardiaque, vasculaire et respiratoire et prévenir les
infections. Dans un tel traitement, it faut suivre différents points qui sont:
- évaluation de la fonction du rein en évaluant les variations des différents
paramétres de fonctionnement rénal;
- méthode Wintervention thérapeutique proprement dite pour remplacer les effets de la
crise rénale (dialyse), pour réduire leur ravage dans I'ensemble de I'organisme et pour
faciliter la guérison clinique (nutrition).
|