Annals
of Burns and Fire Disasters - vol. X - n. 1 - March 1997
DEEP
BURNS OF THE KNEE: JOINT CAPSULE RECONSTRUCTION WITH DERMIS GRAFT
M. Masellis
Divisione di Chirurgia Plastica e
Terapia delle Ustioni, Ospedale Civico, Palermo, ltaly
SUMMARY. Cases are presented of
serious 111 degree deep burns in the knee area, with carbonization of skin tissues, the
rotular apparatus, and muscle and articular tissues, with ample exposure of the femoral
and tibial condyles. In the light of experience acquired both clinically and
experimentally, the authors reconstructed the joint capsule with autologous dermis graft.
This method, by permitting fairly good and rapid articular stability, allows early
mobilization and therefore a favourable modulation of the periarticular scar tissue, with
good recovery of joint movement.
Introduction
One of the advantages of the plastic
surgeon is the ability to identify imaginative alternative solutions to problems of
reconstructive surgery that cannot be solved by normal surgical techniques. The use of
dermis may be included among these solutions, even if its use has had alternating fortunes
in the history of reconstructive plastic surgery.
When in 1987 G. Dogo proposed the use of Padgett's dermotome to remove the whole dermis,
it was possible to overcome the numerous technical and biological problems which
previously had conditioned the use of dermis. With the Padgett dermotome it is possible in
a few minutes to remove a flap of 200 sq cm of dermis, thus permitting immediate repair of
the donor area.
Materials and methods
Histology of the dermis
The dennis is a dense fibrillary connective tissue, also called fibrous connective
tissue, closely related to the epidermis which protects and feeds it. It provides a site
for skin appendages such as hair follicles, sebaceous glands, and sweat glands. The dermis
is conventionally divided into two parts: a) the papillary and periadnexal dermis,
"adventitial dermis", and b) the "reticular dermis". Adventitial
dermis is characterized by thin, haphazardly arranged collagen fibres, delicate branching
elastic fibres, numerous elongated, plump and stellateshaped fibroblasts, abundant ground
substance, and plentiful capillaries, linked to superficial arterial and venous plexuses.
The papillary dermis and the epidermis together form a morphological and functional unit
devoted to the very active metabolic life of the skin. The reticular dermis, the larger
part of the dermis, extends from the base of the papillary dermis to the subcutaneous fat.
It is composed of collagenous fibres arranged in bundles of various thickness and immersed
in a scarce amorphous matrix. The bundles are mostly arranged parallel to the skin surface
in an orthogonal wickerwork. A network of coarse wiry elastic fibres enmenshes the
collagen bundles. In this part of the dermis there are few fibroblasts and blood vessels.
Occasionally, cells of subcutaneous fat can be found.
The fibroblasts are the builder cells of the dermis. They produce all the fibrillary
components, as well as the amorphous matrix.
The collagen of the dermis consists of two different types. Type I forms thick fibres
arranged in a dense orthogonal network in the reticular dermis and seemingly mostly
parallel to the skin surface. Type II collagen is found principally in the adventitial
dermis and consists of thin fibres, loosely arranged.
These fibres are prominent within and beneath the epidermal basement membrane, where they
intermingle with type I collagen fibres.
Immature elastic fibres are aggregates of protein microfibrils grouped cylindrically along
the surface of the fibroblasts. The fibroblast synthesizes a protein, elastin, and
secretes it into the preformed tube of microfibrils.
Collagenous and elastic fibres are closely associated with each other. Collagen presumably
provides the skin with tensile strength, whereas elastin returns the skin to its original
dimension after stretching.
The interstitial substance produced by fibroblasts is composed of amorphous, semifluid
mucoid material. The main components are t , he mucopolysaccharides (hyoluronic acid,
chondroitin sulphate, dermatan sulphate) and cellular elements consisting of fibroblasts,
histiocytes and mast cells, mainly in the perivascular area.
Histology of the articular capsule of
the knee
The articular capsule of the knee consists of a dense fibrous connective tissue in
which thick bundles of collagen fibres in undulating fashion weave in all directions. The
bundles are enveloped by a scarse amorphous matrix in which there are some elastic fibres.
This arrangement offers a high strength to traction and pressure.
Generally the orientation of the bundles is determined by the dynamic strain to which the
articulation is subjected.
The articular side of a capsule is covered by synovial membrane. This membrane consists of
collagen and elastic fibres and it is rich in fibrocytes, adipose cells, and histiocytes.
The surface of the synovial membrane can be enlarged by the presence of synovial villi,
which are rich in vessels. The synovial membrane produces synovia.
The autologous dermis graft
Dermis graft is a free graft containing all the cutaneous strata remaining after
removal of the epidermis, i.e. the deepest strata of the papillary dermis, the reticular
dermis with a minimum quantity of subcutaneous fat, together with the epithelial
components consisting of the epidermic appendages (hair follicles, sebaceous glands and
sweat glands).
The advantages of autologous grafting of the dermis are: the facility and rapidity of
removal thanks to the use of the Padgett dermotome, its resistance, and its limited
post-operative reabsorption, which normally does not exceed 20% of the grafted implant.
The use of dermis autografts, instead of grafts of fascia lata or tendon which previously
were used in reparative operations, especially those requiring considerable resistance to
tensile forces, was introduced by Loewe in 1913 and Rhein in 1914.
Since then dermal autograft has been used in the correction of facial deformity, for knee,
hip and elbow arthroplastics, and to strengthen extra-articular ligaments, e.g. of the
temporomandibular joint.
The use of the dermis has proved to be very effective in the treatment of post-laparotomy
hernias, when it is desired to reinforce the abdominal wall after reconstruction of the
fascial plane.
Studies performed by Peer and Paddock' on fragments of dermis graft have shown that
epidermal residue surviving on the surface of the graft gives rise to the formation of
microscopically sized epidermoid cysts which do not affect the clinical outcome.
Thompsoril, has shown that the sebaceous glands and hair follicles disappear within a
period of between two weeks and two months.
It is probably the hair follicles that cause the formation of the epidermoid cysts. These
cysts, with the progressive increase of the internal tension determined by the epithelial
elements, begin to atrophy and exhibit foreign body reaction accompanied by fibrosis.
The sweat glands survive and function much longer. Their secretions are entirely absorbed
by the adjacent capillaries. No evidence has been found relating their survival to
malignant degeneration.
The pilomotor muscles (arrectores pilorum) survive and the elastic fibres are preserved.
They remain in great numbers arranged as in normal skin.
Technique for removal of the dermis
The dermis removal technique is easily accomplished by using a Padget drum dennotome.
If the blade of the dermotome is regulated to maximum thickness, it is possible to remove
together epidermis and dermis as far as the adipose layer (Fig. 1).
Without detaching the flap adhering to the drum from its connection with the donor area,
the blade is returned to the position of the anterior edge of the drum and regulated again
to a thickness of 0.5 - 0.6 min (Fig. 2).
 |
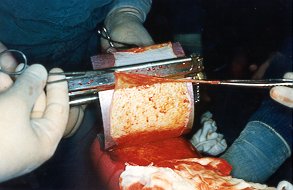 |
Fig. 1
- Dermotome blade regulated to maximum to remove epidermis and dermis. |
Fig. 2
- Dermotome blade regulated to a thickness of 0.5-0.6 mm to separate epidermis from
dermis. |
|
Further cutting separates the
dermo-epidermic flap into two sheets: the epidermic sheet remains attached to the drum,
while the other sheet is free and constitutes the real dermal graft, 0. 14 - 0.6 nim
thick, uniform, and with a surface area of about 200 cm', i.e. equal to that of the
dermotome drum (Fig. 3).
The sheet of epidermis detached from the drum provides an autograft to cover the donor
area (Fig. 4).
 |
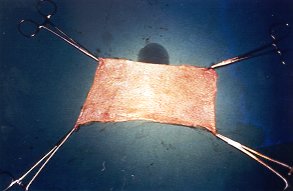 |
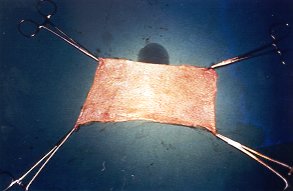
Fig. 3
- The two sheets separated |
Fig. 4 -
The sheet of dermis of 200 cm. |
|
Evolution of the dermis placed
ectopically
The use of dermis to reconstruct the capsular envelope of the knee, metacarpophalangeal
and phalangeal articulations '1042 and Achilles tendons was suggested by confirmation,
after experimentation based on hypothesis, that dermis transferred in ectopic position
reorganizes its structured components with particular advantages for its mechanical
function.A more accurate histological morphological and functional study enabled us to
extend our knowledge of the problem and give it a better biological interpretation and
offered a possible interpretation of the cyto-morpho-architectonic evolution of dermis in
ectopic position. Ten Cate and Freeman identified the role of the fibroblasts in the
repair of slow remodelling cutaneous wounds such as those involving dermis.They described
three separate areas in which fibroblasts behave in a clearly destructive and different
manner in relation to the structured characteristics of the fibroblasts: the area of
preexisting connective tissue, the area of newly formed connective tissue, and the
transition area.The morphofunctional peculiarities of the fibroblasts are the motivation
of the use of dermis in the repair of extensive wounds, although in fact in the
remodelling of the dermis a part is played by all three components of the connective
tissue cells fibres and ground substance. They work together in the remodelling of
collagen during the repair stage, each having a precise role in the final orientation in
the space of the connective fibres that are subjected to precise strains.Ther6 are good
reasons for thinking that both the fibroblasts of the implanted dermis and those of
ectopic areas first cause hydrolysis of the proteoglycans, by means of lysosomial enzymes
acting on the polysaccharide bonds; this is followed by degradation of the collagen
fibres. The purpose of the digestion,of the fibres and the ground substance is the
elaboration of molecules that must adopt a precise spatial organization such that the
definitive collagen fibres may, by interreacting electrostatically with the proteoglycans,
orient themselves according to force lines depending on the outline shape. The production
of fibrils and amorphous matrix is based on a correct balance between absorption on the
one hand and synthesis on the other. This function is performed by the fibroblasts both of
the implanted dermis and of the ectopic area, which take on the ultrastructural
characteristics of active cells. The fibroblasts' phagocytic and synthetic activity
deterinines the area of transition between the preexisting and the nascent connective
tissue. The final arrangement of the aggregated fibres and on the macromolecules of the
ground substance in gel state determines the alignment of the fibres. Thus, the final
remodelling depends on the cell components involved in reabsorption of the fibres,
production of fibres, and ground substance; the arrangement and orientation of the fibres
which, certainly depend on the shape of the outline together with external strain, are
detennined by forces acting both on the fibres and on the macromolecules of the ground
substance.
Clinical cases and results
The dermis was utilized to reconstruct
the articular capsule of the knee, in the event of serious traumas with damage of the
skin, muscles and joint capsule or if there was exposure of the femoral and tibial
condyles.In the case of large trauma of the articular capsule, regardless of the surgical
repair work undertaken, functional recovery is nearly always impaired because of the
formation of a "pannus" above and around the condyles stimulated by prolonged
immobilization, leading to the formation of bone adherences and capsular contraction which
progressively reduce mobility, even causing ankylosis.Rapid reconstruction of the joint
capsule permits an early and moderately good degree of stabilization of the joint, more
rapid mobilization, and more favourable modulation of the particular scar tissue with a
notable degree of articular movement. The trophic function of the dermis is probably
guaranteed by the fact that on the articular face of the re-formed capsule the
reconstruction of the synovial membrane is probably a result of slipping of the synovial
membrane from the residual capsule.
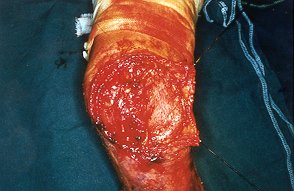
Case I
Woman aged 53 years, who fell onto a brazier in the open containing burning coals, after
loss of consciousnes, remaining for a long time in contact with a source of heat.
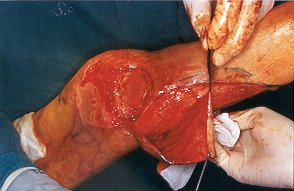
The woman suffered III degree deep burns and carbonization around 3/4 of the knee area and
1/3 of the anterior proximal surface of the leg. Skin, muscles, rotular apparatus and
joint capsule were severely damaged (Fig. 5a).
After initial treatment with chemical escharectomy by means of antiseptic antibiotate
salicylate vaseline"I and subsequent removal, even surgical, of the residual necrotic
tissue of the rotular apparatus and of the articular capsule, the femural and tibial
condyles were amply exposed, appearing to be eroded and damaged by heat action (Fig.
5b).
 |
 |
| Fig. 5a - Knee
and surrounding area on admission |
Fig. 5b
- Exposure fissural and tibial condyles. |
|
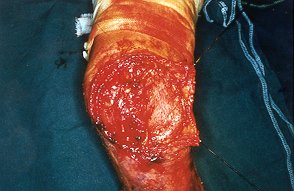
The reconstruction of the capsular
apparatus was achieved by means of dermis.
The sheet of dermis was sutured, with the epideurnic surface towards the joint, to the
residual capsular tissue or to the periosteum by means of Dexon or Vicryl 2/0 stitches. In
this case we used a sandwich of dermis (about 400 em') (Figs. 5c, 5d).
|

|
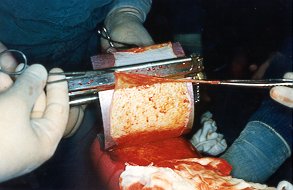
Figs.
5c, 5d - Reconstruction of articular capsule by means of dermis used as a
sandwich. |
|
Skin coverage was ensured by rotation of
an ample fasciocutaneous flap from the posterior face of the leg.
Mobilization and physiokinestherapy began after 7 days. Control at 6 months (Figs. 5e,
5J) and after 4 years (Figs. 5g, 5h).
Case 2
Man aged 79 years, with deep burn of medial surface of the left knee, mediodistal
femoral surface, and medioproximal tibial surface.
After chemical and surgical escharectomy the articular capsule was found to be destroyed
with exposure of the knee articulation (Fig. 6a).
 |
Fig. 6a
- Aspect of knee area after escharectomy. The open articulation. |
|
The surrounding areas were covered by skin
grafts, while the capsular apparatus was reconstructed by means of dermis.
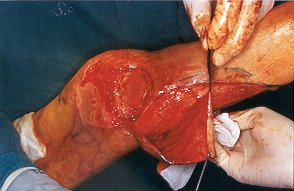
A large fasciocutaneous flaps ensured skin covering (Figs. 6b, 6c).
 |
 |
| Fig. 6b -
Reconstruction of capsular apparatus by means of dermis. |
Fig. 6c -
Skin covering by fasciocutareous flap. |
|
After 7 days the patient began
physiokinesitherapy and after 10-12 days the articular excursion appeared to have fully
recovered (Fig. 6d).
 |
Fig. 6d -
Articular excursion satisfactory
after 10- 12 days. |
|
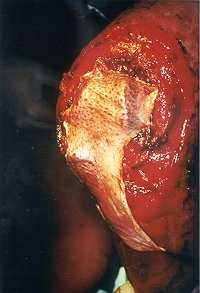
Case 3
Woman aged 75 years with large deep burn of medial surface of proximal third of tibial
region, medial surface of knee, and medial surface of the femoral region.
The patient was admitted to our department from another hospital 45 days after the burn
and after a period time of immobilization (Fig. 7a).
After escharectomy the medial articular capsule appeared totally destroyed with extensive
exposure of the femoral and tibial condyles (Fig. 7b).
 |
 |
| Fig. 7a -
Burned area before complete escharectomy. |
Fig. 7b -
Large exposure of femoral and tibial condyles. |
|
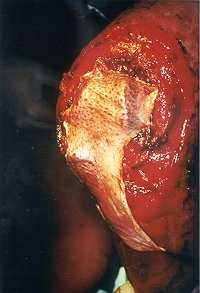
A large sheet of dermis was utilized to
reconstruct the capsular apparatus which was reinforced by two strips of dermis (Figs.
7c, 7d).
 |
 |
| Fig. 7c - The large sheet of dermis
used to recostruct capsular apparatus |
Fig. 7d
- Two strips of dermis were placed to reinforce the reconstructed capsule. |
|
A large fasciocutaneous flaps assured skin
covering The remaining burned areas were covered by skin grafts.
Kinesitherapy began later (after 2 weeks) (Fig. 7e) owing to the protracted previous
immobilization; the recovery was slower and difficult also because of the patient's
advanced age (Figs. 7f , 7g).
 |
Fig. 7e -
Articular excursion after 2 |
|

|

|
| Fig. 7f - A
phase of kinesitherapy |
Fig. 7g - Another
phase of kinesitherapy |
|
Case 4
Child aged 12 with associated injury of contact burn and of the crawling wound in
medial surface of the knee.
After escharectomy there was a large loss of articular capsule with exposure of the
femoral and tibial condyles (Fig. 8a).
 |
Fig.
8a - Large loss of articular capsule
with exposure of condyles. |
|
The reconstruction of the articular
apparatus was achieved with a sheet of dermis reinforced by two strips of the same tissue (Figs.
8b, 8c)
 |
 |
| Fig.
8b - Recostruction of articular apparatus with a sheet of dermis |
Fig.
8c - Scrips of dermis used as reinforcement |
|
Skin coverage was obtained by means of
local skin flaps and a skin graft (Fig. 8d).
 |
Fig.
8d - Before placing skin graft. |
|
There was total recovery of the articulation (Figs.
8e, 8f, 8g, 8h).
 |
 |
| Fig. 8e
- After I year. |
Fig. 8f - Total recovery of
articulation |
 |
 |
| Fig. 8g -
Total recovery of articulation. |
Fig. 8h
- Total recovery of articulation. |
|
Conclusion
We believe that in the case of deep burns
of large joints in which there is destruction of the caDsular envelope the use of
autograft dermis to reconstruct the articular capsule may provide a good solution. The
results obtained in experimental investigations and clinical practice for post-traumatic
lesions enable us to present a method that may serve at least as an alternative surgical
technique to those already in use, which always lead to impairment of functional recovery.
RESUME.
L'auteur présente des cas de brûlure grave de III degré dans le zone du genou, avec
carbonisation des tissus de la peau, de l'appareil rotulien, et des tissus musculaires et
articulaires, avec une ample exposition des condyles fémoraux et tibiaux. Sur la base de
l'expérience acquise cliniquement et expérimentalement, l'auteur a reconstruit la
capsule articulaire utilisant une greffe autologue de derme. Cette méthode, en permettant
une stabilité articulaire acceptable et rapide, facilite une mobilisation précoce et en
conséquence une modulation favorable du tissu cicatriciel périarticulaire.
BIBLIOGRAPHY
- Dogo G.: Trapianto libero di derma net riparo di emie
post-operatocie. Riv. Int. Chir. Plas., 5: 105, 173.
- Mazzoleni E.,Peracchia
A.:L'innestodiden-naneltrattamentodelle ernie post-laparatomiche: risultati chimici
osservati in 60 casi.Riv. It. Chir. Plast., 9: 355, 1977.
- Masellis M., Ferrara M.M., Vitale R.: Laparaplastiche con
innesto ontologo di derma. Arch. Atti XIII Conv. Sec. Siciliana Chir., 389-407: 1979.
- Chiarugi G. "Istituzioni di anatomia dell'uomo",
Società Editrice Libraria, Milano, 1954.
- Ackerman A.B.: "Histologic diagnosis of inflammatory
skin disease", Lea & Febiger, Philadelphia, 1978.
- Rosati P.: "Citologia Istologia", Edi-Ennes,
Milano, 1992.
- Peer L.A., Paddock R.: Histologic studies on the fate of
deeply implanted dermal grafts: observation on sections of implants buried from one week
to one year. Arch. Surg., 34: 268, 1937.
- Thomas N.: The subcutaneous dermis graft. Plast. Reconstr.
Sing., 26: 1, 1960.
- Thompson N.: Transplantation of dermis. In Converse J.M.:
Reconstr. Plastic Surgery, 1, W.B. Saunders, Philadephia, 1977.
- Weeks P.M., Wray P.C.: "Management of acute hand
injuries: a biological approach". Mosby, St. Louis,1976.
- Masellis M., Conte F., Fortezza G.S.: Use of dermis to
reconstruct hand joint capsules. Ann. Plast. Surg., 9: 72,1982.
- Masellis M., Conte F., Fortezza G.S., Ferrara M.M., Benigno
A.: La ricostruzione delle capsule articolari della mano con innesto di derma. Riv. It.
Chit. Plast., 16: 1984.
- Vitale R., Conte F., Masellis M., Raimondi A., De Feo G.,
Ientile A.: L'evoluzione del derma posto in posizione ectopica per ricostruire la capsula
articolare - indagine sperimentale nel coniglio. Riv. It.Chir. Plast., 16: 1, 1984.
- Ten Cate A.R.: Morphological studies of fibrocytes in
connective tissue undergoing rapid remodelling. J. Anat., 112: 401-14, 1972.
- Ten Cate A.R., Freeman E.: Collagen remodelling by
fibroblasts in wound repair: preliminary observations. Anat. Rec., 179: 543-6,1974.
- Masellis M., Valentino B., Ferrara M.M., Vitale R.:
Remodelling of dermal connective tissue in ectopic position, in cutaneous development,
aging and repair. Fidia research series, 18: 74-77, Livinia Press, Padova, Springer
Verlag, Berlin, 1989.
- Weiss L. P., Fawcett D. W.: Cytochemical observations on
chicken monocytes, macrophages and giant cell in tissue culture. J. Histochem. Cytochem.,
1: 47, 1953.
- Donati L. Colonna M., Garbin S., Govom E., Marazzi M.:
"Le ferite e la riparazione tissutale", Linea Farmitalia, B & G Editori,
Verona, 1993.
- Kapandij I.A.: "Fisiologia articolare", Soc.
Edit. DEMI, 1974.
- Masellis M., Vitale R., laia A.: Surgical and chemical
necrectomy: two methods for debridement of burns. Riv. It. Chir. Plast., 13: 1722,1981.
- Masellis M., Vitale R., Giammanco A., Antona A.: The
association of salicyfic vaseline with antiseptics and antibiotics in the topical
treatment and debridement of burns. Bull. and Clin. Rev. Burn Injur., 1: 46-7, 1984.
- Masellis M.: Association of salicylic vaseline with
antiseptics or antibiotics in topical treatment of burns. In "Care of the burn
wound", Karger, Basel, 1985.
This paper was received on 23 September 1996.
Address correspondence to: Dr. M. Masellis
Div. Chit. Plastica e Terapia delle Ustioni,
Ospedale Civico, Via C. Lazzaro, 90145 Palermo, Italy. |
|