Annals of
Burns and Fire Disasters - vol. XII - n° 4 - December 1999
EXTENSIVE KELOIDS IN THE AURICLE - SURGICAL TREATMENT BY MEANS OF AUTOLOGOUS
GRAFTS
Masellis M., Ferrara M.M.
Division of Plastic Surgery and Plastic Surgery, Civic Hospital, Palermo, Italy
SUMMARY. This
article considers two cases of keloid formation in the auricle. Keloids usually affect the
dermis and are characterized by the presence of thick collagenous fibres of vitreous and
hyalinized aspect. Some related fibroblasts are also present. ln the early stages the
formations tend to be more vascularized, especially in peripheral zones, while in the more
mature phase they are more hyalinized. The removal of an ample keloid, as in the cases
reported here, and the repair of an exposed area with a dermo-epidermal full-thickness
skin graft cause both general and specific modifications in the healing process. The
removal of an ample keloid, as reported here, and the repair of an exposed area with a
denno-epidermal full-thickness skin graft cause both general and specific modifications in
the healing process. The surgical techniques employed are described and the various
problems involved are considered. Although only two cases are considered, the experience
obtained makes it possible to repropose the treatment of keloids with the free skin graft
technique, at least in cases located in the auricle, without the supplementary assistance
of medical or physical therapy.
Introduction
Keloids are generally
defined as abnormal fibrous proliferations of the dermis. Clinically they appear as
nodular, frequently lobulated, solid masses extending laterally into healthy tissue. They
grow continuously but intermittently, and show no evidence of significant regression.
During the initial phase of development and during the period of active growth, the
lesions are reddish or violet, with modest vascularization and small blood vessels visible
beneath the skin covering.
During the phase of development and in periods of quiescence, keloids are less tense and
vascularized, but remain raised and more compact than tiormal tissue. Unlike hypertrophic
scars, they do not cause retraction.
The commonest age for the onset of keloids is between 15 and 45 yr. They are more frequent
in females and a certain degree of familial heredity has been reported. Blacks are the
most frequently affected race, in particular Africans and East Indians.
The onset can be triggered by a skin lesion even of limited dimensions such as an acne or
smallpox pustule, a wart, an insect bite, a vaccination scratch, a tattoo, a
electrocauterization, or a surgical operation.
Following a surgical operation the onset is late, with a marked tendency to recidivation
after excision.
The typical features of keloids, i.e. their nonregression in time, tendency to
recidivation, and spreading to normal tissue, are useful in diagnosis for differentiating
from hypertrophic scars.
These features will however appear in time and thus it is not always possible to make an
early clinical differentiation between a hypertrophic scar and a keloid.
Some body areas show a particular predisposition for keloid formation. These are mostly
concentrated in the upper half of the body, for example the head, neck, thorax, shoulders,
and arms. In these specific areas the most commonly affected are the earlobes, the
pre-sternal area, and the deltoid region. Keloids are also sometimes seen in the umbilical
and pubic zones.
Certain conditions, in addition to endogenous factors, facilitate the onset of keloids,
e.g. the local tension to which a wound suture is subjected, the orientation of a lesion
in relation to lines of cutaneous tension, the presence or absence of infection and
foreign objects (hair, endogenous keratinized material, etc.), and second-intention
healing.
Histology
The histological picture
of the keloid is well defined. The condition usually affects the dermis and is
characterized by the presence of thick collagenous fibres of vitreous and hyalinized
aspect. A limited number of related fibroblasts are present, embedded in a rich matrix of
mucinous material.
In the early stages the formation tends to be more vascularized, especially in peripheral
zones; in the more mature phase the appearance is more hyalinized, with a lower vascular
component and an almost scar-like appearance. The overlying epidermis may appear normal or
acanthoid.
The fibroblasts present a clearly evident Golgi complex and a well-developed rough
endoplasmic reticulum.
In fresh keloids, chemical analysis indicates the presence of a disproportionate increase
in the synthesis of collagen, protocollagen, and fibronectin compared with hypertrophic
scars and mature keloids, confirming that the anabolic phase in keloids is exaggeratedly
accelerated.
Under the polarized-light microscope the birefrangent collagen fibres appear yellow-green
in colour and composed of thick fibres arranged in parallel or irregular bundles. No
myofibroblasts are present.
Materials and methods
We observed two cases of
extensive keloid formations involving both auricles in one case and the left auricle only
in the other.
The patients were subjected to general anaesthesia, followed by complete removal of the
keloid formations peripheral to the healthy skin tissue down to the perichondrial planes.
The exposed area was reconstructed with a free full-thickness skin graft taken from the
inguinal fold and fixed with 4/0 silk suture and normal containment dressings, which were
removed on day 7.
The follow-up was scheduled for 3-6-12-24 months.
No pharmacological or physical treatment was performed.
Clinical cases
Case I
A.A., female, aged 33 yrs
Anamnesis: the patient reported that 3 yr previously (1990) she had been subjected
to otoplasty surgery for the correction of the "satyr" look of both her
auricles.
The operation was performed with exposure and modelling of the helix by a marginal
incision. This left a scar which in the next few months developed into a clearly keloid
formation.
Two years later (1992; the patient was subjected to a further unspecified operation for
removal of keloid tissue in both auricles.
Also in this case the scars developed into keloids, which the patient presented when she
came to our observation in 1995.
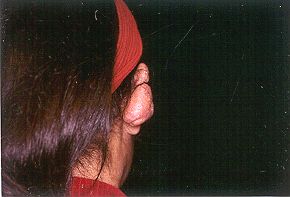
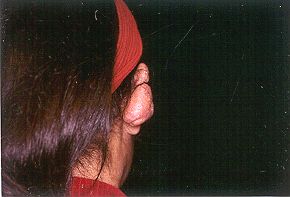
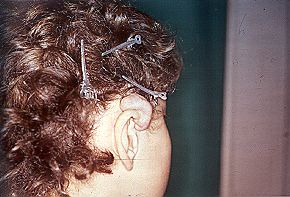
Right auricle
Mass of clearly keloid tissue involving nearly the entire lateral face of the helix,
the antihelix forward and as far as the edge of the concha and down as far as the upper
edge of the lobe, extending over the border of the auricle in nearly all the medial face.
In places the mass was 4-5 cm thick.
The mass was reddish, lumpy, and in places grooved, with irregular margins at its base. It
was itchy and painful (Figs. 1, 2).
 |
 |
Figs. 1, 2 - Keloid in right auricle. |
|
Left
auricle
Also in this auricle the mass was large in extent, involving a stretch of the upper
edge of the helix, the descending edge, the groove of the helix, and nearly all the medial
face. Thickness in lower part, 3-4 cm (Figs. 3, 4).
 |
 |
Figs. 3, 4 - Keloid in left auricle. |
|
Clinical
treatment
The clinical picture was similar to that described in the previous case.
On 1 July 1996 we removed the keloid masses in both auricles as far as 1/2 cm, on the
edges of the healthy skin tissue, to the depth of the perichondrium.
The exposed areas were covered using full-thickness free skin grafts taken from the left
inguinal region.
The histological examination of the pieces removed yielded the following results:
"The neoformations are characterized by the presence at chorion level of thick
bundles of collagen. These are intensely eosinophil and irregular in arrangement. The
bands are immersed in a fair-sized matrix rich in acid mucopolysaccharides. The periphery
of the lesion is the site of marked vascularization, and the overlying skin shows a modest
degree of atrophy. Conclusion: the histological picture is compatible with a diagnosis of
keloid."
Follow-up was performed at 3-6-12-24 months.
The follow-up examinations indicated progressive consolidation of the skin graft and a
phase of mimimal retraction followed by a phase of distension and softening. There were no
signs of keloid recidivation (Figs. 5-8).
Examination
of the donor sites did not reveal any sign of scar pathology (Fig. 9).
 |
Fig.
9 - Normal scarring process in inguinal donor site. |
|
Case 2
R.A., male, aged 11 yr.
Anamnesis: the parents reported that at the age of 4 yr (1991), following an insect
(tick ?) bite in the medial face of the right auricle, a progressive scarring reaction
began, of hypertrophic-keloid appearance. This was surgically removed at the age of 7 yr
(1993).
The histological examination of the part removed was not available.
Recidivation occurred some months later, and surgical removal was performed in January
1994.
The histological examination reported: "Diffuse myofibroblast proliferation of
the dermis with highly vascularized collagenization. Picture compatible with hyperplastic
scar lesion".
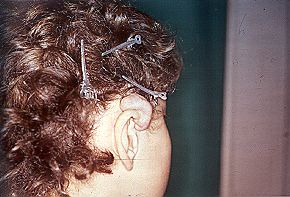
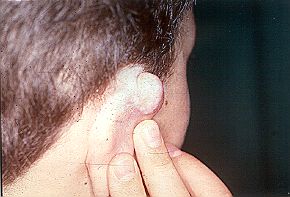
An objective examination performed in 1997 indicated a clearly fibrous area of tissue
involving the edge of the radix and the ascendant and upper part of the helix. This
occupies the lateral face of the triangular fossa.
In the medial face the upper third of its surface (1-2 cm thick) is lobulate in appearance
and reddish in colour, hard in consistency, and often painful and itchy (Figs. 10, 11).
 |
 |
Figs. 10, 11 - Keloid in upper third of auricle. |
|
Surgical
treatment
On 1 July 1997, radical excision was performed on the keloid mass as far as the
peripheral planes and 1.5 cm on healthy skin tissue.
The exposed area was covered with free full-thickness skin graft removed from the right
inguinal fold.
Histological examination: exuberant tissue neoformation of mesenchymatic origin
giving a "collagenized" aspect to both papillar and reticular dermis. ne
connective. bundles in these districts were massed, with either a parallel arrangement in
relation to the major axis of the epidermis or an irregular presentation, appearing to be
mainly composed of hyalinized collagen fibres of acidophilic appearance. The interstice
contains random aggregates of fibroblasts and myofibroblasts in a matrix containing foci
of Alcian-positive mucinous material. Moderate presence of vascular structures surrounded
by reticules of argentophile fibres. The epidermal covering is adequately represented in
every district and is often acanthotic.
The picture was that of a "nodular keloid" in a histologically florid phase.
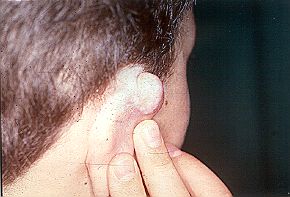
Follow-up was performed at 6-9-12 months. The postoperative course up to 12 months showed
progressive consolidation of the skin graft in the various phases of retraction,
distension, and softening. There were no signs of recidivation (Figs. 12, 13).
 |
 |
Figs. 12, 13 - Follow-up after one yr |
|
The
inguinal donor area healed normally with no sign of scar pathology (Fig. 14).
 |
Fig.
14 - Inguinal donor site after one yr. |
|
Considerations
The removal of an ample
keloid,. as in the cases reported here, and the repair of an exposed area with a
dermo-epidermal full-thickness skin graft cause both general and specific modifications in
the healing process.
In cases of extensive wounds with loss of cutaneous substance, it as known that healing
occurs by second intention through processes of angiogenesis, granulation, fibroblast
migration, collagen synthesis, the appearance of myofibroblasts, and modelling of the
scar.
During this phase extrinsic and mechanical infective and iatrogenic factors, together with
intrinsic dysmetabolic and hormonal factors, impair the process of the regulation of
collagen production and degradation. This may trigger pathological mechanisms that affect
and/or delay wound healing.
The application of a skin graft, with the transfer to the exposed area of epidermis and
derrms and all its mesenchymal components, causes modifications in the healing process.
These determine the success of graft take in the successive phases of serum imbibition,
vascularization, and neoangiogenesis.
It is likely that the fibroblasts of the grafted dermis and those of the recipient area
together initially activate hydrolysis of the proteoglycans by means of the lysosomial
enzymes, which act on the polysaccharide connections and then cause degradation of the
collagen fibres.
The purpose of the digestion of the fibres and ground substance is to process molecules
that have to adapt themselves to a precise organizational pattern in which the final
collagen fibres interact electrostatically with the proteoglycans and arrange themselves
according to the lines of force acting in the area.
The synthesis of fibrils and amorphous substance is regulated by correct balancing between
absorption and synthesis.
This function is performed equally by fibroblasts in the receiving area and in the grafted
dermis, which take on the ultrastructural characteristics of active cells.
Phagocytic activity and that of fibroblast synthesis determine an area of transition
between the connective tissue already existing and that newly formed.
The final positioning of the aggregated collagen fibres and of the macromolecules of the
ground substance in a state of gel determines the alignment of the fibres.
The remodelling of the tissue is thus related to the activity of the cell components
involved in the re-absorptior of the fibres and in the production of fibres and grounc
substance. The composition and orientation of the fibre depend on the forces that act on
the fibres and macro molecules of the matrix.
With regard to the specific problem of keloid formation it has been shown that besides the
familial element there is the finding that the fibroblasts of patients suffering from
keloids are phenotypically different from those of healthy persons. This suggests that the
pathology may have genetic cause.
Keloid fibroblasts are thought to present a reduction in the normal feedback of the
regulation of production of the extracellular matrix. These fibroblasts would appear to
respond more energetically to the action of growth factors, even if the obligatory
affinities and densities of the receptors are identical to those of normal cells.
The observation in our cases that the graft donor area did not in time manifest any keloid
transformation suggests a non-generalized tendency to keloid formation reserved to certain
specific areas, such as the very common forms frequently encountered in the sternal
region, the auricles, the deltoid region, and the abdominal area.
These areas would thus appear to present a particular "field activity" related
in some way to the characteristics of the skin, an immunological organ that is the site of
histocompatibility antigens.
There are however other factors that should not be neglected, as stressed by various
researchers, such as tension on the wound, the position of the wound in relation to skin
orientation, the presence of infection, and healing by first or second intention.
It may also be supposed that, following dermoepidermal graft, biological activity in loco
is modified by the input of mesenchymal cell elements and in particular of fibroblasts
from other districts. In particular, the fibroblasts transferred with the dermis, which
are activated by the graft trauma and are possibly numerically superior to those present
in the recipient area, an area exposed down to the perichondrial stratum, would appear to
dominate the regulatory feedback activity of production and degradation of the collagen
fibres and the ground substance, thus restoring a condition of normal healing.
It should not be forgotten that the treatment of keloids by excision and repair with skin
graft has been proposed by various researchers but the results obtained have been judged
unfavourably as the recidivation rate was 46%.
In modem practice surgical excision is associated either with pharmacological treatment,
e.g. cortisones, antiphlogistics, and interferon, or with physical treatment, e.g. elastic
compression, radiotherapy, and plesiotherapy administered pre- or post-operatively.
Conclusions
The limited number of our
cases does not permit us to draw definitive conclusions. The experience obtained in the
treatment of the two patients described does however enable us to repropose the treatment
of keloids with the free skin graft technique, at least in cases localized in the auricle,
without the supplementary assistance of medical or physical therapy.
RESUME. Les
Auteurs présentent deux cas de la formation de chéloïdes dans l'auricule.
Généralement les chéloïdes se produisent dans le derme et sont caracterisées par la
présence de fibres collagéneuses épaisses d'aspect vitreux et hyalinisé. On note aussi
la présence de fibroblastes connexes. Dans les phases précoces les formations sont
généralement plus vascularisées, particulièrement dans les zones périphériques,
tandis que dans les phases plus matures elles sont plus hyalinisées. L'ablation d'une
chéloïde diffuse, comme dans les cas décrits par les Auteurs, et la réparation d'une
zone exposée moyennant l'emploi d'une greffe cutanée dermoépidermique à toute
épaisseur provoquent des modifications générales et spécifiques dans le processus de
la guérison. Les Auteurs décrivent les techniques chirurgicales et les problèmes qui
peuvent se produire. Bien qu'ils considèrent seulement deux cas l'expérience gagnée
leur permet de reproposer le traitement des chéloïdes moyennant la technique de la
greffe libre, au moins dans les cas situés dans l'auricule, sans l'assistance
supplementaire de la thérapie médicale ou physique.
BIBLIOGRAPHY
Converse J.M.: "Plastic Surgery", W.B. Saunders Co., Philadelphia, London,
Toronto, vol. 1: 157-63, 424-30, 1977.
Enzinger F.M., Weiss S.W.: "Soft Tissue Tumors", Mosby, St. Louis,
193-9, 1995.
Donati L., Colonna M., Garbin S., Govom E., Marazzi M.: "Le ferite e la riparazione
tessutale", Linea Formitalia Bi&Gi, Ed. Tori, Verona, 1993.
Elder D., Elenidsas R., Jaworsky C., Johnson B., Jr: "Histopathology of the
skin", Lippincott, Raven, 8th ed., 881-7, 1997.
Ehrlich H.P., Desmouliere A., Diegelmann R., Cohen LK., Compton C.C., Garner
W.L., Kapanci Y., Gabbiani G.: Morphological and immunochemical differences between
keloid and hypertrophic sear. Am. J. Path., 145:105-13, 1994.
Lawrence W.T.: Physiology of the acute wound. Clinics in Plast. Surg., 25:
321-40, 1998.
Nwomeh B., Yager D.R., Cohen LK.: Physiology of the chronic wound. Clinics in Plast.
Surg., 25: 341-56, 1998.
Steed D.L.: Modifying the wound healing response with exogenous growth factors. Clinics
in Plast. Surg., 25: 321-40, 1998.
Hunt T.K.: "Ferite cicatrizzanti e ferite infette", Liviana Editrice,
Padua,1993.
Montandon D., D'Andiran G., Gabbiani G.: Wound contraction and epithelialization.
Clinical and experimental studies. Clinics in Plast. Surg., 4: 325-46, 1977.
Su C.W, Alizadeh K., Boddie A., Lee R.C.: The problem scar. Clinics in Plast. Surg., 25:
451-65, 1998.
Masellis M., Valentino B., Ferrara M.M., Vitale R.: Remodelling of connective tissue in
ectopic position - Cutaneous development, aging and repair. Abatangelo G., Davidson J.M
(eds), Fidia Research Series, Liviana Press, Springer-Verlag, 1989.
Masellis M.: Deep burns of the knee: Joint capsule reconstruction with dermis graft.
Ann. Burns and Fire Disasters, 10: 3-11, 1997.
Rosati P.: "Citologia, Istologia". Ed. Hermes, Milan, 1987.
Masellis M., Ferrara M.M., Vitale R.: Vaste neopasie del volto: riparo mediante innesto
libero di cute. Riv. It. Chir. Plast., 10: 18595, 1978.
Cohen I.K., Diegelmann R.F.: The biology of keloid and hypertrophic scar and the
influence corticosteroid. Clinics in Plast. Surg., 4: 297-9, 1977.
Larrabee W.F., East C.A., Jaffe H.S., Stephenson C., Peterson K.E.: Intralesional
interferon gamma treatment for keloids and hypertrophic scars. Arch. Otolaryngol Head Neck
Surg., 116: 1159-63, 1990.
Pitter B., Rubbia-Brandt L., Desmouliere A., Sappino A.P., Roggero R., Guerret S.,
Grimaud J.A., Lacher R., Montandon D., Gabbiani G.: Effect of y-interferon on the clinical
and biologic evolution of hypertrophic scars and Dupuytren's disease: An open pilot study.
Plast. Reconstr. Surg., 93: 1224-35, 1994.
| This paper was received on 28
April 1999. Address correspondence to:
Prof. Michele Masellis
Divisione di Chirurgia Plastica e Terapia delle Ustioni
Azienda Ospedale Civico
Via C. Lazzaro, 90128 Palermo, Italy.
Tel.: 0039 091 6822860; fax: 0039 091 596404; e-mail: mbcpa@cres.it |

M.B.C.
The Mediterranean Burns Club
|
The International Symposium and Course
on Burns and Fire Disaster Management
(3rd Jerusalem Meeting)
Jerusalem,
Israel, February 13 -16, 2000 |

|
L.B.A.
The Israel Burn Assoiciation |
|

Endorsed by the I.S.B.I.
International Society for Burn Injuries
|
|
Symposia
- Symposium: Local antibacterial treatment of burns;
- Symposium: Methodology in burn research: models of burns
(means, etiology, assessment of depth and size, criteria, statistical considerations,
treatment, scars, etc.)
- Policy development: triage and burn treatment in mass
casualty
Courses
- Splints and pressure garments: hands on sessions for
physical therapists and occupational therapists
- Local wound care: means and technologies (for nurses and
physicians)
- Burn prevention: techniques and employment of local
resources
A. Burns and the community
Prevention
Mass casualty and catastrophe management
B. Acute phase
Resuscitation and metabolism
Pain control and psychological aspects
Burn wound management
Infections
C. Late phase
Reconstruction and scar modulation
Contact
the Secretariat if you require any additional information or assistance.
Please address all correspondence to:
"Burns and Fire Disaster Management"
P.O. Box 50006, Tel Aviv 61500, ISRAEL
Tel: 972 3 5140018/9; Fax: 972 3 5175674 or 972 3 5172484
E-mail: medburn2000@Kenes.com
Web site: www.kenes.com/burn2000 |
|