Annals of
Burns and Fire Disasters - vol. XIII - n° 1 - March 2000
TREATMENT OF POST-BURN DEFECTS IN THE UPPER
MEMBER
Martinez-Sahuquillo Marquez J.M., Jimenez
Còrdoba G., Martinez-Sahuquillo A.
Department of Plastic Surgery and Burns,
Virgen Macarena University Hospital, Seville, Spain
SUMMARY. Defects in the burned upper member vary in relation to the
following factors: the severity of the burn, inadequate management, and general or local
complications. Accurate treatment can reduce the impact of the defects. Injuries in the
joints, the arms, and the hands are considered. Various combinations of injuries are also
described. The successive steps in the reconstruction process are presented.
The upper member is
of great importance as it holds and sustains the hand, which is - after the brain - our
body's most perceptive organ.
The hand and the arm are a physiological kinetic unit, joined together functionally,
biologically, and mechanically from the fingertips to the shoulder - hence the functional
and aesthetic importance of the correction of defects in the upper member in order to
recover the normal mobility of its joints as well as its appearance.
Burn-related defects in the upper member vary as a function of the following factors:
- the severity of the burn - except in the
case of firstdegree bums, there is always some functional or aesthetic defect, however
well they have been treated
- inadequate management of the burn
- general or local complications of the burn
These defects can be
minimized by appropriate management. This includes early removal of scars, the use of free
skin grafts to cover affected areas, accurate positioning of the member, active and
passive rehabilitation, the use of Job compressive garments, and the careful monitoring of
treatment during the acute phase of the bum.
The treatment of post-burn defects involves surgery as well as rehabilitation. Surgery
aims at repairing damaged structures. In general tenns this phase should begin as soon as
possible - ideally when the scars are stabilized, which usually occurs between 6 and 24
months post-trauma. It is however advisable to operate earlier in the case of growing
children, whose joints suffer great stress and may be displaced, and in whom the defect is
still expanding and may affect functionality. During this period of time, the joints
should be moved active and passively; continuous pressure should be exercised on the skin
tissue, and topical or intra-intestinal cortisone should be prescribed.
In general, and before treatment of the bum, all elements that have been affected,
especially those involving joints and the hand, should be clinically and radiologically
examined in order to assess the state of the muscles, tendons, blood vessels, and nerves.
This provides thorough knowledge of the elements that have to be repaired and helps to
establish the most appropriate management plan.
Before any attempt is made to repair the defects, the surface and the deeper layers of the
scarred tissue must be removed, the vital elements must be freed, and a generous area of
skin next to the defect must be lifted in order to evaluate the actual loss of tissue and
the elements that need to be repaired. Haemostasis must be meticulous and the retraction
of the vital elements, as also manipulation of the joints. must be performed with utmost
care in order to prevent further damage.
To repair loss of skin in joint areas, it is advisable to use free skin grafts and skin
flaps (Figs. 1, 2).

|

|
| Fig. la - Retractile scar in armpit and anterior side of
elbow. Liberation of armpit and repair with free skin graft. Two Z plasties were performed
in the elbow. |
Fig.
1b - Result 8 months later |
|

|
| Fig. 2a - Retractile scars in both |
Fig. 2b - Post-operative result. armpits and elbow.
Repair with skin flaps. |
|
If
possible, flexible skin should be used for placement on the deep planes, in order to avoid
secondary retractions. It should be sufficiently cushioned to withstand pressure and
scratches and to allow further interventions. These features can be found only in skin
flaps and in some free skin grafts. Free skin grafts should not however be used when the
removal of scar tissue would expose vital elements such as nerves, blood vessels, and
tendons, a not infrequent occurrence in the arrnpits and flexible areas of the elbow and
the back of the hand. Another advantage of using flaps is their optimal elasticity, which
allows total recovery of active and passive joint movements with adequate post-surgical
rehabilitation - there are no limitations from the cutaneous point of view.
Regarding the techniques used to repair the cutaneous cover, the only limitations on the
management of these conditions are basically the size, depth, and location of the defect
and the state of the adjacent tissue. The easiest procedure must always be used: removal
and direct suture; free skin grafts; and adjacent, distant, fasciocutancous, myocutancous,
and free skin flaps.
Owing to the anatomical and functional characteristics of the different areas of the upper
member, we have classified post-burn injuries following Mir y Mir: in the joints, in both
arms, and in the hands.
Injuries in the joints
and in both arms
The correction of injuries in the armpit, elbow, and wrist is of great importance
owing to the functional disabilities they may cause. Injuries in the armpit may lead to
inadequate abduction, elevation, ante-position, and retrocession of the arm, thus limiting
hand mobility. Injuries in the elbow and the wrist impede flexor extension and pronation
of the forearm and hand. When bums in the upper member affect the armpit or its anterior
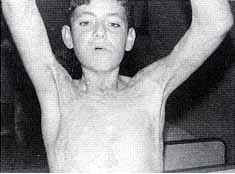
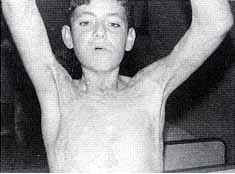
surface they cause retractions or contractions (Fig. 3).
 |
 |
 |
| Fig.
3a - Retractile scar on anterior side of arm |
Fig.
3b - Repair with local flaps |
Fig.
3c - Result one yr later |
|
When they
affect the posterior surface they cause chronic ulcerations in the acromion and the
olecranon, adherence to tendons near the wrist and the back of the hand, and the
lack-of-skin syndrome. Defects in isolated areas of the shoulder and in the arm and
forearm indirectly affect the joint areas, hindering normal functioning. The elbow is
considered to be the most likely area for post-burn heterotopic calcifications.
These consequences range from simple lineal retractile scars that affect normal
functioning of the joint to large contractions that interfere with movements of the joints
or are distiguring.
For lineal retractions we use skin flaps, chiefly simple or multiple Z-plasties. These are
easy to implement and provide tissue similar to the tissue we wish to correct, the scar is
less visible, and the operation can performed rapidly. Its only inconvenience is its
indications. The combination of flaps and free skin grafts succeeds in solving most joint
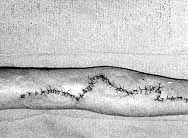
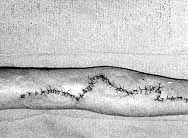
contraction problems (Fig. 4).

|

|
Fig. 4a - Retractile scar on
anterior side of elbow. Wide removal, liberation of adjacent tissues, and repair with free
skin graft. |
Fig. 4b - Result 8 months later. |
|
We use free
skin grafts to repair defects in both arms, for large branchiothorax retractions, for
those located on the extension surfaces of the joints and the back of the hand, and for
those located in scarred surfaces in the flexion areas where no vital elements are
exposed. Free skin grafts have the disadvantage of causing secondary retraction, thus
necessitating protracted immobilization if performed in a flexion area.
If vital elements are exposed, we use adjacent skin flaps, either alone or combined with
free skin grafts or distant flaps. For retractions affecting the neck, arm, and thorax in
which a large scar joins the arm to the neck and thorax, once the sear has been removed we
repair the area using skin grafts and branchial flaps and the lateral thorax with the
upper pedicle. These defects can now be repaired with scapular and parascapular
fasciocutaneous flaps - mainly the latter as they are longer and can provide more tissue.
The hypogastric flap irrigated by the tipper epigastric artery is very mobile, which makes
it very useful for repairing defects on the front and back surfaces of the elbow (Figs. 5,
6).

|
Fig.
5a - Retractile scar in the elbow. |

|

|
Fig.
5b - Removal of scar. Tendons and vessels exposed. Correction with epigastric
flap. |
Fig.
5c - Result 6 months later. |
|
|

|

|

|
Fig.
6a-d - Retractile scar in elbow, with exposure of olecranon, preventing flexion.
Repair with epigastric flap, offering good functional results. |
|
Injuries
in the hands
The repair of post-burn defects in the hand is a challenge for the plastic surgeon,
not only because of the difficulties involved in the reconstruction itself but also
considering how rewarding reconstruction is for the patient. Bums are perhaps the greatest
of physiological tragedies for the professional and functional development. of the
individual with regard not only to the person's working activity but also to the more
social and intimate sphere. Any defect in this field can cause important psychological
problems that may give rise to psychopathies affecting the individual's mental and
emotional integrity and creating economic and social disorders.
Owing to the numerous elements that can be involved, it is difficult to classify post-burn
injuries in the hands. For simplicity's sake, it can be said that burns affecting the
anterior surface of the hand affect only its surface, the subcutaneous cell tissue, and
the aponeurosis because of the thickness of the skin in this area, and cause retraction in
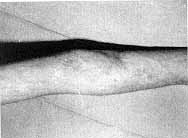
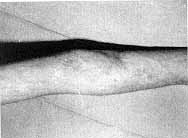
the palm of the hands and the fingers, with retractile interdiggital scars (Fig. 7).

|
![Fig. 7b - Hand ferule a] temating with active joint mobilization.](../images/gr0000051.jpg)
|

|
Fig. 7a - Claw-hand. Liberation of fingers and
reconstruction of commissures with skingrafts |
Fig.
7b - Hand ferule a] temating with active joint mobilization. |
Fig.
7c - Result 6 months late |
|
In more
severe cases there can be claw-hand, club-hand, and total or partial amputation. Burns on
the back of the hand can affect the tendons with luxations in the interphalangeal joints
of the fingers.
There can be other different combinations, such as the presence of some fingers in flexion
and others in extension, as well as total or partial amputation, longitudinal scar band,
traumatic syndactylies caused by interdigital scars, mainly in the proximal phalanges,
joint deformities, painful scars in the finger tips, ectopia of the fingers, adherences
and tendon rupture (especially in the extensors and rarely in the flexors), carpal tunnel
syndrome, corns and deformities in the nails, etc. Before repairing any such lesions, it
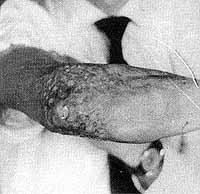
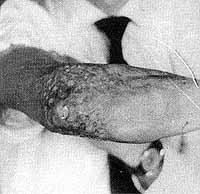
is essential to know the state of the skin, tendons, joints, vessels, and nerves (Fig.
8).

|

|

|
| Fig. 8a - Large defect in hand. |
Fig. 8b - Removal of scar tissue and liberation of
fingers and commissures. |
Fig.
8c - Repair with threequarters thickness free skin graft. The first three fingers
were liberated and the fourth was later amputated, achieving a good holding function and
mobility of the other fingers. |
|
It is also
very useful to assess the mobility of the joints and to carry out x-rays and bone
tomographies, vascular studies, and electromyograms, as all these procedures provide a
general idea of the elements needing to be repaired and help to prepare the most
appropriate plan. In most cases, more than one surgical intervention will be necessary.
The first step is to reconstruct the cutaneous layers. If the scar contracture is
immature, it is advisable to use compressive dressings. If the scar contracture is
stabilized, surgery is the alternative, using the techniques mentioned.
To reconstruct defects in the tendons, joints, and other elements, it is indispensable to
have a good cutaneous layer (Fig. 9).
 |
 |
Fig. 9a, b - Thumb adhering to palm of hand with
loss of first commissure. Total liberation of thumb and repair of palm and anterior
surface of finger with groin flap. |
|
The
techniques used to repair the skin depend on the size and depth of the wounds. We use
Z-plasties to treat retractile scar bands, free skin grafts (preferably full or
three-quarters thickness), and skin flaps. The groin flap, irrigated by the superficial
iliac artery, is very suitable for reconstructing defects in the hand as it provides a
great deal of thin skin and is very versatile. The following procedures are also
recommended: Z-plasty combined with skin grafts, simple island flaps, neurovascular
pedicular island flaps, and free flaps.
Tenotomies, osteotomies, arthrodesis, sutures, tendon and nerve transplants, amputations,
etc., along with dynamic splints, compression and, above all, adequate rehabilitation
enable us to obtain functional solutions for various severe post-burn defects that affect
the elements of the hand.
RESUME. Les
défauts du membre supérieur brûlé varient selon les facteurs suivants: la sévérité
de la brûlure, la gestion inadéquate, et les complications générales et locales. Un
traitement soigné peut réduire l'effet des défauts. Les Auteurs considèrent les
lésions des articulations des bras et des mains. Ils considèrent en outre diverses
combinations des lésions. Les phases successives du procès de reconstruction sont
présentées.
BIBLIOGRAPHY
Benaira F.: Enfoque global del tratamiento
de las quemaduras. In: Coiffman, "Cirugfa Plàstica, Reconstructiva y
Estética", MassonSalvat., Barcelona, 443-96, 1994.
Franco Diaz A.: "Manual de Tratamiento de las Quemaduras". Liade, Madrid,
1985.
Gabilondo F.J.: Secuelas de Quemaduras. Enfoque terapéutico. XXXIV SEPRE Congress,
Mapfre, Madrid, p. 46, 1999.
Garcia Torres V.: "Quernaduras.
Tratamiento de Urgencia". Duphar Farmaceutica, Madrid, 1993.
Garcia Torres V., Gomez Bajo G.I., Leyva
Rodriguez F.: Presente y pasado de las quemaduras. XXXIV SEPRE Congress, Mapfre, Madrid,
p. 44, 1999.
Lazo Zbikowski M.: Contracturas en lexiôn
postquemaduras. International Burns Congress, Buenos Aires, 1984.
Martfnez Sahuquillo A.: Secuelas
postquemaduras de las manos. Inf. Medico-Terapeutica, 7: 404-15, 1959.
Martfnez Sahuquillo A.: Sistematica en el
tratamiento de las quernaduras. Sevilla Médica, 5: 21-23, 1970.
Martinez Sahuquillo A., Morales Lupiafiez
F., Gonzalez Peirona E.: Cicatrices retràctiles postquemaduras de axila y codo. Traum.
Cir. Rehab., 9: 167-74, 1979.
Martfnez Sahuquillo A.: Quemaduras. In:
Curso sobre Urgencias en Cirugfa Plastica, Colegio Oficial de A.T.S. y D.E. de Huelva,
10517,1987.
Martinez Sahuquillo A.: Quemaduras. In: "Actualizaciôn 1 y Il Curso sobre
Urgencias en Cirugfa Plàstica", Duphar Farmaceutica, Madrid, 137-51, 1989.
Mir y Mir L.: "Fisiopatologia y
Tratamiento de las Quernaduras y sus Secuelas", Scientifico Médica, Barcelona, 1969.
Mir y Mir L.: Plastias en Z. In: Coiffman,
"Cirugfa Plàstica, Reconstructiva y Estética", Masson-Salvat., 348-58, 1994.
Mirabet L "Quemados. Manual prActico". Quiles, Valencia, 1979.
15. Nappi J.F., Lubbers L.M., Carl B.A.: Composite tissue transfer in burn patients. Clin.
Plast. Surg., 13: 137-42, 1986.
Rebello C., Lo-King-Tien S., Lion P.M.:
Secuelas de quemaduras. In: Coiffman, "Cirugfa Pldstica, Reconstructiva y
Est6tica", Masson-Salvat., 604-11, 1994.
Robson M.C., Hayward P.G.: Principios de
cirugfa reconstructiva. In: Bendem A., Linares H.A., Benaim F., "Tratamiento de las
quemaduras", Interamericana, Madrid, 444-54, 1996.
Salisbury R.E., Marville N., Dingeldein
G.P.: Tratarniento en la quemaduras. In: "Planteamiento interdisciplinario",
MassonSalvat., Barcelona, 1986.
Santoqui-Melani C.: Quemaduras. Reflexiones generales. In: Coiffman, "Cirugia
Plastica, Reconstructiva y Estetica", Masson, 439, 1994.
Silverberg B. et al.: Microsurgical reconstruction for the electrical and deep thermal
injury. Proc. Am. Burn Assoc., 17: 129-32, 1985.
Wang X.: Early vascular grafting to prevent
upper extremity necrosis after electrical bums. China Med. J., 97: 53-9, 1984.
Vilar Sancho B.: Principios generates del
tratamiento de las secuelas de quemaduras. Rev. Esp. Cif. Plast., 1: 2-3, 1968.
This paper was presented at
the First International Congress on
the Prevention and Reduction of Disasters in
the Mediterranean held in Valencia, Spain, in May 1999.
Address correspondence to:
Dr J.M. Martinez-Sahuquillo Marquez
Department of Plastic Surgery and Burns
Virgen Macarena University Hospital, Seville, Spain. |
|













![Fig. 7b - Hand ferule a] temating with active joint mobilization.](../images/gr0000051.jpg)





