Annals of the MBC - vol. 3 - n' 2 - June 1990 FOREARM FASCIOCUTANEOUS FLAPS FOR COVERAGE OF DEFECTS AROUND THE ELBOWOsman OR, Houtah A.M. Plastic Surgery Unit, Department of Surgery, Faculty of Medicine, AI-Azhar University, Cairo, Egypt SUMMARY. This work details our experience in 9 patients with contracted elbow, for reconstruction of the defects after release of bum cicatrix, utilizing a proximally based forearm fasciocutaneous flap. The results were promising, with regain of full range of movements in a short post-operative period. Introduction Skin defects around the elbow
represent a difficult reconstructive problem for plastic surgeons. Many reports have been
published on methods of reconstructing this defect, with skin grafts, pedicle flaps (2),
muscle and musculocutaneous flaps (4) and free (8) vascularized tissue. Fasciocutaneous
forearm transposition flaps with their enhanced fascial vascular contribution has provided
a useful means of achieving satisfactory coverage for such defects (1, 7). Patients Nine patients with post-burn contracted elbow were submitted to this study. Their age, sex and contracted size are summarized in the Table. Operative technique After excision of the scar and release of the antecubital contracture, the defect is measured and the flap designed on the medial aspect of the forearm (1) (over the flexor muscle group) or on the lateral aspect of the forearm (over the brachioradialis muscle) and, if necessary, extending over the extensor surface of the forearm. The size and location of the defect, and the possible are of rotation will dictate flap design. The length to width ratio should not be more than 3 to 1. The medial, distal and lateral skin incisions are carried down through the underlying deep fascia of the forearm. Dissection of the flap starts from its distal part, elevating it from the underlying muscle carefully in order to preserve musculocutaneous perforators at the base of the flap. Dissection stops as soon as ample mobility has been achieved, to allow transposition of the flap to the defect. Narrow flap donor sites may be closed primarily by approximation, but larger donor sites will require coverage with partial -thickness skin grafts.
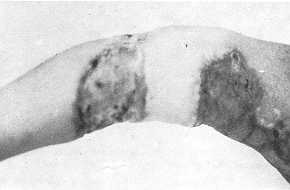
Results In all patients, the flaps healed
perfectly in 10 days. The largest flap in this series measured 15 x 5 em (patient No. 1)
and the smallest 3 x 6 em (patient No. 4, Table). Representative examples are shown in
Figs. 1, 2, 3 and 4). Discussion Improper early management of burned upper limbs is still the main cause of scar contractures around the elbow. Skin defect around the elbow, particularly after release of contracture, with exposed vital structures, presents the surgeon with a challenging reconstructive problem. Many procedures have been described for coverage of the elbow region. Skin grafts require a well-vascularized bed and long-term splinting to prevent the risk of recontracture. Muscle flaps and musculocutaneous flaps (4) are not an option because of their functional deficits. Pedicle flaps require a staged procedure and long,periods of immobilization and hospitalization. Free flaps (8) have also been employed to cover such defects. Such flaps require not only a suitable healthy patients but also microvascular (3) expertise and special facilities, and they should be reserved for large complex defects that are not amenable to local flap closure.
The extensive continuing anatomical study
(5, 6) of the vascular territories of the forearm skin and the demonstration of the
clinical applicability of the proximally based fasciocutancous forearm flaps provided a
highly efficient means for coverage of skin defect around the elbow. The flap can be
elevated on the medial aspect of the forearm (over the flexor muscle group) or on the
lateral aspect (over the brachioradialis muscle). The flap can safely encompass up to
one-half of the forearm skin.
RESUME. Les Auteurs décrivent leur expérience chez 9 brûlés avec contraction du coude pour ce qui concerne la reconstruction des défauts qui se sont produits à la suite de la décharge de la cicatrice, avec l'emploi d'un lambeau fasciocutané de l'avant-bras avec base proximale. Les résultats ont été positifs et ils ont permis aux patients de recouvrer toute la gamme des mouvements après une courte période postopératoire. BIBLIOGRAPHY
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||