Annals of the MBC - vol. 3 - n' 3 -
September 1990
RISK FACTORS IN THE
CRITICAL BURN PATIENT
Santos Heredero F.X., Garcia Torres V.*, Herruzo R.*,
Fernàndez Delgado J.*
Burn Unit, Hospital del Aire
* Burn Unit, Hospital "La Paz", Madrid, Spain
SUMMARY. 194 burned patients
were studied to find out the influence of three risk factors, previous pathology (PP),
inhalation syndrome (IS) and ventilatory support (VS), on their evolution. The mean
mortality rate in patients with PP was 58.7%, more than twice the overall rate (25.2%).
The higher mortality appeared in neurological (83%) and epileptic (80%) patients. Patients
with PP developed twice as many complications as those without pre-existing disease. A
history of toxic or hot fumes inhalation (with or without clinical correlation) was
recorded in 42.5% of cases. This increased mortality to 50% (7% without IS). In this group
of patients, complications were three times as frequent as in IS-free cases [ARDS (95%),
sepsis (81%) and respiratory infections (80%)]. A total of 73 patients (37.6%) required
VS. This therapy exponentially increased infective complications as long as the mechanical
ventilation was maintained. It is concluded that an exhaustive exploration and anamnesis
is mandatory to discover previous diseases and inhalation of fumes during the accident.
Once the presence of PP or IS is confirmed a number of therapeutic steps should be taken
to prevent the expected high number of complications and to reduce the death risk.
Usually the evaluation of the critical bum
patient is based upon the age, burned surface area and depth of the wounds. According to
all or some of these parameters, the "probit" scales are elaborated in an
attempt to predict the mortality rate of these patients (1). Nevertheless, there are other
risk factors directly related to the evolution of the bum disease. In an attempt to find
out which are the most expressive factors, we considered a list of them (Table 1) (2).
In this first interpretation of the
results obtained, we present the following risk factors:
- previous pathology
- inhalation syndrome
- ventilatory support.
Material and methods
During the period from January 1986 to
December 1987, 194 patients were included in the study. The mean age was 39.9 (+/- 1.5)
years. The sex distribution was 139 (71.6%) males and 55 (28.4%) females.
The mean burned surface area was 39.6%
1.5). 41.7% of the wounds were subdermal and 58.3% dermal.
Table 2 shows the distribution according to the bum mechanism. It should be pointed that
almost 75% of the bums were caused by flame. This fact could explain the great incidence
of inhalation injuries that will later be considered.
The frequency of each risk factor was studied in the group and then a statistic analysis
was accomplished using chi-square and Fisher tests.
Results
1. Previous pqthology
A total of 86 patients (44.3%) were
found to suffer from one of the following types of disorders: alcoholism, cardiological,
neurological, psychiatric, parenteral drug-addiction, pneumological, metabolic, epileptic,
others. The distribution rates are shown in Table 3.
With regard to the influence of pre-existing disease on the mortality rate, Table 4 shows
the significant elevation of the death rate in patients with some particular previous
pathologies. The mean mortality rate in patients with previous pathology is 58.7%,
compared to an overall mortality of 25.3%.
5 out of the 6 patients with neurologic previous disease died, i.e. 83%. These five
patients were more than 65 years old: age was thus an added risk factor in th , eir
neurological disease. Almost the same rate occurred in the epileptic patients. In contrast
to the neurological patients, three out of the four deaths occurred in patients aged
between 25 and 45 years old. In these cases age was therefore not an added risk factor.
Another more and more frequent event in our Bum Units is the presence of burned patients
with a history of addiction to parenteral drugs. This factor should alert us when
receiving this kind of patient. They are likely to have a worse evolution than average
cases.
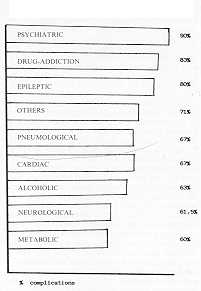
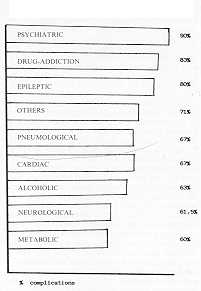
The presence of a previous pathology not only increases the mortality rate but also
obscures the general evolution of the patient and causes a higher rate of complications.
Out of a total number of 86 patients with previous diseases, 60 (70%) developed some kind
of complication during their hospitalization. This contrasts with only 35% of
complications in patients without any previous disease. In other words, the patients with
previous pathology develop twice as many complications as those without pre-existing
disease. Table 5 shows the complication rates with each type of previous disease. We can
find some kind of complication in almost all the patients (90%) with psychiatric
disorders. As in relation to the death rate, drug addicts show a very high rate of
complications (83%). The complications considered in this study are: general infection
(with or without sepsis), respiratory infection, cardiac disorders and adult respiratory
distress syndrome (ARDS). In all groups of patients with previous pathology, the most
frequent complication was ARDS, except for patients with pre-existing cardiac disease, who
most frequently developed some kind of cardiac complication.
2. Inhalation Syndrome (IS)
Inhalation injury appears in three
basic forms, alone or in combination: carbon monoxide poisoning, direct heat injury, and
chemical damage (8). In our series 82 patients '(42.5%) inhaled some kind of toxic or hot
fumes during the thermal accident. This was more frequent in bums caused by flame (64
cases, 78%) occurring in a closed space. These data agree with the most reliable series
(4, 5, 6, 7).
A relation was found between IS and the mortality rate. Out of the 82 patients who inhaled
toxic fumes, 41 died, representing a mortality rate of 50%. Among the other 45 cases in
whom smoke inhalation was not reported, there were only 8 deaths (mortality 17%). The
death causes were distributed as follows; sepsis 16 cases (39%), ARDS 13 cases (36.5%),
cardiac disorders 5 cases (12.1%), others 5 (12. 1 %). These rates are not far away from
the 45 -78% reported by various authors (8, 9, 10).
The above data clearly indicate that the inhalation of toxic fumes is one of the most
important risk factors preventing the survival of burned patients. Smoke inhalation has
multiple clinical effects: upper airways oedema, tracheo-bronchitis, pulmonary
insufficiency, atelectasis, bronchiolitis, ARDS, etc. In our series we consider a patient
to have IS only on the basis of the accident history, independently of the clinical
repercussion of the fact.
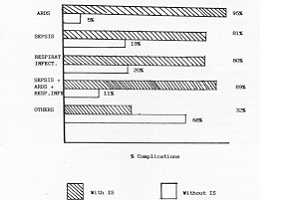
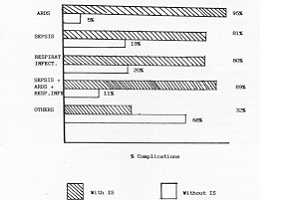
In an attempt to find out the influence of IS on the clinical evolution of the burned
patient, the complications of such patients were recorded. Table 6 shows the most
important complications and their relation with the presence or absence of IS. Among the
82 patients with IS, 70 of them (85%) developed some of the recorded complications. On the
other hand, among the 112 patients without IS, only 28 of them (25%) had a complicated
evolution. These data indicate that patients who inhaled smoke develop three times as many
complications as those who are IS-free.
Table 1 Potential risk factors
- - Age
- - Burn mechanism
- - Sex
- - Inhalation of hot or toxic fumes
- - Burn surface area
- - Bum depth
- - Debridement date
- - Type of debridement
- - Ventilatory support
- - Previous pathology
- - etc.
- - Flame
- - Electricity
- - Gas explosion
- - Scald
- - Chemical
|
149 (74.5%)
21 (10.8%)
19 (9.3%)
7 (3.6%)
3 (1.5%) |
|
Table 2 Burns
mechanism |
|
- - Alcoholic
- - Cardiac
- - Neurological
- - Psychiatric
- - Parent. drug addict.
- - Pneumological
- - Metabolic
- - Epileptic
- - Others
|
19 (22%)
15 (17%)
13 (15%)
10 (12%)
6 (6%)
6 (7%)
5 (6%)
5 (6%)
7 (8%) |
|
Table 3 Previous
pathology N' 86 (44.3%) |
|
| Prev. pathology |
Deaths / Total |
% mortality |
Pneumological
Epileptic
Alcoholic
Metabolic
Neurological
Drug addiction
Psychiatric
Cardiac
Others |
5 / 6
4 / 5
13 / 19
3 / 5
7 / 13
3 / 6
5 / 10
6 / 15
3 / 7 |
83%
80%
68%
60%
54%
50%
50%
40%
43% |
|
Table 4 Mortality
in patients with previous pathology |
|
Complications related to infection and,
pulmonary function were most frequently recorded in patients with IS. As many as 95% of IS
patients developed ARDS, and 80% some other kind of respiratory disease. This means that
almost all the patients with a history of toxic inhalation will have their lung function
compromised. But more serious than this is the finding of 89% of IS patients with ARDS,
respiratory infection and sepsis, who developed a critical status that in the majority of
cases needed intensive respiratory care.
Other complications occurred only in 32% of IS patients.
In conclusion, patients with a history of toxic inhalation, with or without clinical
repercussion on admission, will develop pulmonary conditions and will be infected.
3. Ventilatory support
A total of 73 patients required
mechanical ventilation, representing 37.6% of the series. This ventilatory support was
maintained for I to 7 days in 31 patients, for 7 to 14 days in 29, and for more than 15
days in 13 patients.
Out of the 121 patients without ventilatory support, only I died (0.9%), but out of the 73
mechanically ventilated patients, 49 died (67%). This first finding directly associates
mechanical ventilation with mortality (chi-square 42.273, p <0.001).
If we correlate the need of ventilatory support with the incidence of complications, the
data are more significant. Table 7 shows the complication rate in patients with and
without mechanical ventilation. The first conclusion obtained from these data is that
complications are directly associated with mechanical ventilation (p<0.001). Infections
are the most frequently reported complications (34%), including sepsis, wound infection
and respiratory infections. ARDS, directly or indirectly related to respiratory infection,
also has a high rate in patients under mechanical ventilation (50%).
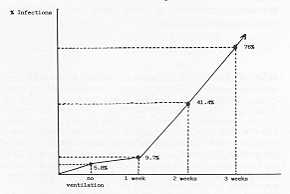
If we draw a graph showing the evolution of infective complications in relation to the
duration of mechanical ventilation, we obtain the result shown in Fig. 1. Infective
complications are more frequent, in absolute figures, during the second week of mechanical
ventilation. In relative terms, there is a progressive increase of complications as the
number of days under mechanical ventilation increases. In the second week, 12 out of the
29 patients developed infection (41.4%). With ventilations longer than 15 days we recorded
10 infections out of 13 patients (77%). There is therefore an exponential increase of
infective complications in relation to the duration of mechanical ventilation (Fig. 1).
Hansbrough et al. (11) notice that altered cell-mediated immunity accompanies hyperbaric
oxygen exposure, and the immunosuppressive effect is exerted through inactivation of
macrophages. This could be the origin of some of the infective complications observed in
patients under mechanical ventilation with high oxygen concentrations.
4. Correlation between previous
pathology and inhalation syndrome
Among the 86 patients with previous
pathology, 49 (57%) inhaled toxic fumes during the accident. Only 33 patients among the
108 without previous; pathology inhaled smoke (30.5%). This means a double incidence of IS
in patients with previous disease if compared with the rate obtained in the group without
any pre-existing pathology.
Table 8 shows the incidence of IS among patients with previous pathology. It should be
noticed that 100% of the epileptic patients inhaled fumes. Four of them sustained the
accident in direct relation with an attack, losing consciousness and inhaling smoke for
some time. The fifth epileptic patient was burned while sleeping and until he awoke and
escaped he had been inhaling for several minutes.
Drug addiction is another previous pathology with a very high incidence of IS (83.3%). It
is probably related to the poor level of self-control of these patients, who are not able
to escape rapidly from the fire, and are thus exposed to toxic fumes for a long time.
The eight patients with neurological disease who inhaled smoke were all more than 65 years
old. This explains the high incidence of IS in patients with ischaemic cerebral disease.
Discussion
Alcoholism, a very frequent pathology
among our patients, is present in 22% of the cases, and this group had a mortality rate of
58.4%. The altered liver function and associated disorders could be responsible for the
poor response to the "general bum syndrome.
Probably age ( >65 years) is responsible for the high mortality (83%) of the patients
with pre-existing
 |
 |
| Table 5 Complications
in patients with previous pathology |
Table 6 Complications
in patients with IS |
|
Table 7 Complications in patients under
mechanical ventilation
| PP |
PP
/ IS |
% |
| Epileptic |
5 / 5 |
100% |
| Drug addiction |
6 / 5 |
83.3% |
| Neurol ogical |
13/ 8 |
61.5% |
| Psychiatric |
10 / 6 |
60% |
| Metabolic |
5 / 3 |
60% |
| Pneumological |
16 / 3 |
50% |
| Cardiac |
15/ 7 |
46.7% |
| Alcoholism |
19/ 8 |
42% |
| Others |
6 / 4 |
67% |
| Total |
86 / 49 |
57% |
|
Table 8 IS in
patients with previous pathology (PP) |
|
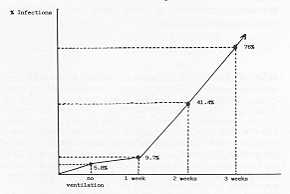 |
Figure 1 Relation
between days of ventilation and infective complications disease. |
|
Drug addiction seems to be a more and more frequent
problem in Bum Units. These patients, with or without AIDS antibodies, had 50% mortality
and some kind of major complication in 83% of cases. Special attention should be paid to
the high incidence of infection in these patients, which seriously obscures the general
evolution of the bum syndrome.
Burns caused by flame provoke inhalation of toxic fumes in 78% of cases. This increases
the mortality rate to seven times the expected rate for patients without inhalation. The
cause of this increase is the presence of three times as many complications in these
patients. Almost 100% of the overall IS cases develop either pulmonary or infective
complications. Although IS in our series includes only a history of smoke inhalation, with
or without clinical correlation, ARDS was developed by 95% of cases and respiratory
infection by 80%. These data show the great influence of fumes inhalation on ventilatory
function. It means that every patient should be checked for direct or indirect signs of
smoke inhalation. These signs mainly are: singed nasal vibrissae, carbonaceous sputum,
rales, rhonchi and, in particular, all facial bums caused by flame. The patient or
accompanying persons should also be interrogated for details of the accident: mechanism,
open or closed space, loss of consciousness, etc. Even if there are no signs of IS on
admission, but suspicion of it is amply justified, all measures should be taken to prevent
and treat the more than probable complications (10, 12). These measures include thorax
X-ray control, ventilatory function monitoring, and blood gas analyses, together with the
possibility of oxygenotherapy, intubation, and ventilatory support with PEEP (13) at the
first sign of respiratory distress. We believe that the standardizing of an intestinal
decontamination protocol helps in preventing a great number of autoinfections. If this is
true for all kinds of critically burned patients, in those with IS it should be mandatory,
considering their high risk of serious infective complications.
If IS is a demonstrable risk factor for burned patients, another factor is frequently
present: the necessity of mechanical ventilatory support. This measure was needed in 89%
of the IS patients. Mortality rates increased to almost 10 times those obtained in
patients without ventilatory support. This spectacular increase in mortality is directly
related to an exponential rise of complications in relation to the number of days under
mechanical ventilation. The confirmation of this finding is one of the most evident
results of our series. The longer the mechanical ventilation was maintained, the higher
the risk of infective complications. This would seem to be due to the presence of a
permanent new colonization pathway, restriction of mucociliar bronchial function, etc.
Special attention should be focused on keeping the best lung function during respiratory
support, in order to minimize areas of poor ventilation, which is a very frequent cause of
respiratory infection. If I patient is not able to maintain an acceptable air flow
spontaneously, he should be immediately sedated and the ventilator should be used to
expand the lungs adequately. In such cases, frequent oropharyngeal cultures, as well as
from the tubes system, should be performed, in order to identify possible colonizations
Three pre-existing diseases appeared to have the most important relationship with IS:
epilepsy, drug addiction and neurological syndromes. This finding was easily explained by
the actual characteristics of the first two pathologies and by the age ( 65 years) and
partial disability of the neurological patients. Nevertheless, patients with decreased
mentation, such as that produced by drug overdose, alcohol intoxication or neurological
disease, frequently experience smoke inhalation injury because , f prolonged exposure to
the offending gases. Prim respiratory disease and cigarette smoking compound the effects
of inhalation injury and may transform a relatively insignificant injury into a fatal
disease.
RÉSUMÉ. Les
Auteurs ont étudié 194 patients brûlés pour établir l'influence sur leur évolution
de trois facteurs de risque, C'est-à-dire la pathologie précédente (PP), la syndrome
d'inhalation (SI) et le support ventilatoire (SV). Le taux moyen de mortalité chez les
patients avec PP était 58,7%, plus de deux fois le taux complessif (25,3%). La mortalité
majeure se vérifiait chez les patients neurologiques (83%) et épileptiques (80%). Les
patients avec PP ont développé des complications deux fois plus fréquemment que les
patients sans PP. Il y avait une histoire d'inhalation de fumées toxiques ou chaudes
(avec ou sans corrélations cliniques) en 42,5% des cas, ce qui augmentait la mortalité
à 50% (7% sans SI). Chez ce groupe de patients les complications étaient trois fois plus
fréquentes que chez les cas sans SI [ARDS (95%) ' infection générale (81%),
infections respiratoires (80%)]. 73 patients (37,6%) ont eu besoin de SV. Cette thérapie
augmentait en manière exponentielle les complications infectieuses tant que durait la
ventilation mécanique. Les Auteurs concluent qu'il faut absolument exécuter une
exploration et une anamnèse exhaustive pour établir soit les maladies précédentes soit
l'inhalation de fumées pendant l'accident. Une fois confirmée la présence de PP ou de
SI, il faut prendre des mesures thérapeutiques pour prévenir les nombreuses
complications prévisibles et pour réduire le risque de la mort.
BIBLIOGRAPHY
- Garcia Salvatierra B. et al.: Determinaci6n de la
probabilidad de muerte en el enfermo quemado. XX Reunion de la Sociedad Espafiola de
Cirugia Pldstica. Le6n 13-14 October, 1989.
- Santos Heredero F.X. et al.: Factores de riesgo en
el quemado critico. XX Reuniòn de la Sociedad Espahola de Cirugia Plàstica, Leon 13-14
October, 1989.
- Madden M.R., Finkelstein J.L., Goodwin C.W.:
Respiratory Care of the Bum Patient. Clinics in Plastic Surgery: 13, 1: 29-39, 1996.
- Foley F.D., Moncrief J.A., Mason A.D. Jr.: Pathology
of the lung in fatally burned patients. Ann. Surg., 167: 251-264, 1968.
- Di Vicenti F.C., Pruitt B.A. Jr., Reckler J.M.:
Inhalation injuries. J. Trauma, 11: 109-171, 1971.
- Shook C.D., MacMillan B.G., Alteimer W.A.: Pulmonary
complications of the burn patient. Arch. Surg., 97: 215-224, 1968.
- Silverstein P., Dressler D.P.: Effect of current
therapy on bum mortality. Ann. Surg.: 171: 124-129, 1970.
- Sochor F.M., Mallory G.K.: Lung lesions in patients
dying of burns. Arch. Pathol., 75: 91-96, 1963.
- Wroblenski D.A., Bower G.C.: The significance of
facial bums in acute smoke inhalation. Crit. Care Med., 7: 335-338, 1979.
- Zawacki B.E., Jung R.C., Joyce J., Rincon E.: Smoke,
bums and the natural history of inhalation injury in fire victims. Ann. Surg., 185:
100-110, 1977.
- Hansbrough J. F., Piancentine J.G., Eiseman B.:
Immunosuppresion by hyperbaric oxygen. Surgery, 87: 662, 1980.
- Putman C.E., Loke J., Matthay R.A., Ravin C.E.:
Radiographic manifestations of acute smoke inhalation. Amm. J. Roentgenol., 129: 865-870,
1977.
- Davies LX, Poulton T.J., Modell J.H.: Continuous
positive pressure is beneficial in treatment of smoke inhalation. Crit. Care Med., 11:
726-729, 1983.
|