Annals of the MBC - vol. 4 - n' 1 -
March 1991
PERMANENT SKIN
HOMOGRAFTING BETWEEN MONOZYGOTIC TWINS
Bejar J.M., Jul C., Alonso F., Garcia Masclevall M.D.*,
Gabilondo F.J.
Service of Plastic Surgery and Burns Center, Cruces
Hospital, Baracaldo (Vizcaya), Spain * Service of Imunology, Cruces Hospital
SUMMARY. The problem of
permanent skin coverage in patients with bums has still not been solved. There are two
principal lines of research regarding this. One of these is the use of hom6grafts from
cadavers in the coverage, using immunosuppressive drugs to prevent rejection. The other is
the development of techniques for tissue culture, which has opened new possibilities. This
paper shows the results obtained by performing homografts of skin on a severely burned
patient, taken from a monozygotic twin. The results obtained indicate what could be
achieved after the problems which both lines of investigation still present have been
overcome.
Introduction
The problem of permanent skin coverage
in severely burned patients is a question which, despite progress in the last few years,
has still has aot found a definitive solution. One line of work consists of temporary
coverage by means of homografts from cadavers and the use of immunosuppression to prevent
rejection, as advocated by Burke (1) and Achauer (2). The other is the development of
techniques for tissue culture which has made possible the achievement of sheets of
keratinocytes from the patient himself, which can be used for permanent recovering, as in
Gallico (3) and Cuono (4). However, the problems of both solutions are still in the
investigation and improvement phase.
In this paper we present the results obtained in a severely burned patient who underwent a
skin transplant from his monozygotic twin. This is the perfect case for carrying out a
homograft without requiring the use of immunosuppression to guarantee the viability of the
graft, which acts as if one were dealing with the ideal case for using the techniques of
skin culture to provide dermis and epidermis with all the cells normally present in it.
Case report
A 40-year-old patient was brought into
our Unit having suffered a road accident. On admission he had second- and third-degree
bums caused by fire in approximately 55% BSA, with deep bums in approximately 40% BSA (for
distribution see Fig. 1).
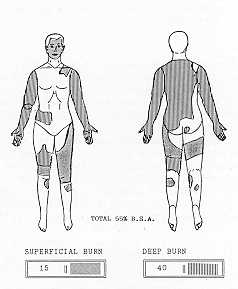 |
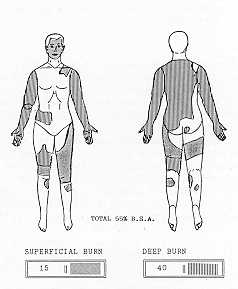
Fig. I Body
surface area bum estimation chart of patient when he was admitted to the Bum Unit. |
|
The patient had a more than 80% death
probability, according to the formula of Zawacki (Fig. 2) (5).
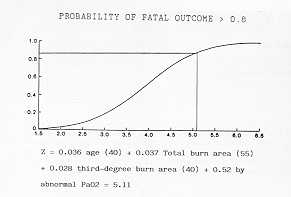 |
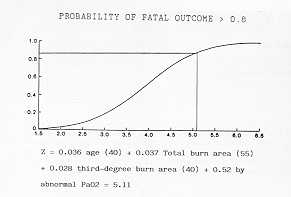
Fig. 2 Probability
of fatal outcome of patient according to the Zawacki probit. |
|
He was submitted to the usual protocol of
treatment in our Unit with fluid replacement as in the Parkland plan. Decompressive
escharotomies were also carried out in both upper extremities. After the shock phase we
began programme of administering calories with related nutrition, as his calorie needs,
according to the Curreri formula, were 4,000 calories a day.
The patient was submitted to two surgical debridements, in both of which tangential
excisions were performed. In the first debridement (day 5 post-bum) we excised 18% of the
body surface, grafting 10% of it. The patient developed a septic process which delayed the
second operation, performed on day 19 post-bum. On this day we excised the rest of the
bums, except in the area of the back, and grafted approximately 25% of the body surface in
total, performing the grafts previously mashed. 20% of the body surface was grafted with
split-thickness skin graft coming from a twin brother from whom the skin was removed (from
the back), after an immunological check had been performed (Tab. 1).
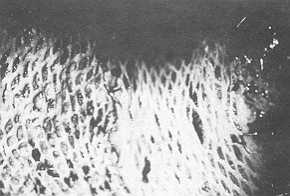 |
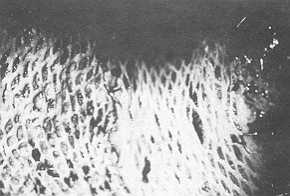
Fig. 3 A
recent aspect of meshed graft taken from donor twin and placed over wound on left elbow of
burned twin. |
|
All the meshed grafts took without any
problem (Fig. 3). Consequently, the patient was placed on an air-fluidized bed to help the
epithelialization of the burns on his back. Complete epithelialization under these
conditions was achieved on day 36 post-bum. On this day the patient left the Bums Unit to
begin rehabilitation and pressure therapy (Figs. 4 and 5).
 |
 |
| Fig. 4 Meshed
grafts taken from donor twin and placed in their new body (6 months after injury). |
Fig. 5 The
two twin brothers. On the left (with beard) donor twin. On the right burned twin. |
|
The donor areas of the twin were closed
completely by day 7 without demonstrating any problems up to the present time (Fig. 6).
 |
Fig.
6 A view of donor site (back) of donor twin, 6 months after graft was removed. |
|
Discussion
We have studied the literature and
this appears to be the I I th case of a skin transplant between twins in order to heal
bums in one of them: Converse in 1947 in a leg burn (6), Bradford in 1953 in a patient
with 60% BSA (7), Cox in 1965 in two cases with 50% BSA and 30% BSA (8), Patterson in 1960
in a patient with 680/rBSA (9), Herron in 1967 (10), Kortholm in 1968 in a case with 59%
BSA (11), Niederhuber in 1970 in a case with 50% BSA (12), Westerveld in 1986 (13), and
Coenen in 1990 in a patient with 50% BSA (14).
As we can see, our patient was within the group of patients with some possibility of
recovery following the scheme published by Muir, Barclay and Settle in 1987 (15). This
possibility of recovery is influenced by the percentage of bums which are cured by the
patient's own skin, the number of surgical operations needed for total recovery, and the
increase of the exposed area caused by the removal of skin for grafting. These last two
factors momentarily aggravate the situation of the patient, by increasing the exposed area
and augmenting the loss by evaporation from the wound and the risk of infection.
Technically this case could have been resolved with conventional treatment, but the fact
that the vatient had a monozygotic twin offered us a quicker and more effective solution,
and with less risk for the patient (by avoiding the need to increase the exposed area by
taking grafts).
The possibility of using completely histocompatible skin (or if this is not possible, of
preventing its rejection) is the aim of the two lines of investigation to which we
referred in the introduction. This case presents characteristics in its resolution which
could be shared by both lines; on the one hand, a homograft was carried out, and, on the
other, the behaviour of the homograft (which took completely, without rejection) is
similar to that of cultured skin.
The evolution of this case underlines the importance of the investigation of the
phenomenon of rejection and its avoidance, together with the transcendental importance for
this type of patient of the possibility of growing complete skin (dermis and epidermis
with their melanic cells), and of having it available whenever necessary.
It is impossible to know the greater life expectation in such a case of the availability
of a donor of isogenic skin, though we can say that it obviously diminished the risk of
death. Likewise, when problems of rejection and of skin culture are solved, we will have
to correct the life expectation tables for these patients.
Conclusions
We have presented this case because of
the peculiarity of the use of a twin brother in its solution. This shortened the patient's
hospitalisation time, and reduced the risk of mortality and morbidity.
This will help us to compare the results that we will obtain in our patients when the
problems of rejection are solved and the transplant of laboratory-grown skin has become
routine in Bum Units.
RESUME. Le probl6me de la couverture cutan6e
permanente chez les patients br6l&s West pas encore r6solu. 11 y actuellement deux
principales lignes de recherche. Lune regarde 1'emploi des allogreffes cadav6riques pour
la couverture, associ6 A I'administration des immunosuppresseurs pour pr6venir le rejet;
I'autre conceme le d6veloppement des techniques de la culture cellulaire, qui a ouvert de
nouvelles possibilit6s. Les Auteurs d6crivent les r6sultats obtenus avec I'application,
chez un grand br616, des allogreffes cutan6es donn6es par son jumeau monozygote. Ces
r6sultats indiquent ce qui sera possible d'obtenir apr6s la solution des probl&mes
6tudi6s par les deux lignes de recherche.
BIBLIOGRAPHY
- Burke J,F., Quinby W.C., Bondoc C.C. et al.:
Immunosuppression and temporary skin transplantation in the treatment of massive third
degree bums. Ann. Surg.: 182-183, 1975.
- Achauer B.M,, Hewitt C.W., Black K.S. el al.:
Long-term skin allograft survival after short-term cyclosporin treatment in a patient with
massive bums. Lancet, 14: Jan. 4 1986.
- Gallico G., O'Connor N.E., Compton C.C. et al.:
Permanent coverage of large bum wounds with autologous cultured human epithelium. N. Engl.
J. Med., 311: 448, 1984.
- Cuono C., Langdon R., McGuire J.: Use of cultured
epidermal autografts and dermal allografts as a skin replacement after bum injury. Lancet,
1123: May 17, 1986.
- Zawacki B.E., Azen S.P., Imbus S.H. et al.:
Multifactorial probit analysis of mortality in burned patients. Ann. Surg. 189: 1, 1979.
- Converse J.M., Duchet G.: Successful homologous skin
grafting in a war bum using an identical twin as donor. Plast. Reconstr. Surg. 2: 342,
1947.
- Blandford S.E., Garcia F,A.: Successful homogeneous
skin graft in a severe bum using an identical twin as donor. Plast. Reconstr. Surg. 11:
31, 1953.
- Cox P.A., Fredricks S.: Successful homografting
between identical twins. Plast. Reconstr, Surg., 18: 141, 1956.
- Patterson JR: Homografting between identical twins,
Plast. Reconstr. Surg., 25: 510, 1980.
- Herron P.W., Marion L.F.: Homografting in the
treatment of severe burns, using an identical twin as a skin donor. Pac. Med. Surg., 75-
4, 1967.
- Kortholm B.: Transplantation between monozygotic
twins. Scand. J. Plast. Reconstr. Surg., 2; 64, 1968.
- Niederhuber J., Feller I.: Permanent skin
homografting in identical twins. Arch. Surg., 100: 126, 1970.
- Westerveld A. W., San& E.W., Klasen H.J.:
Successful treatment of a severely burned elderly patient with homografts from her
identical twin sister. Br. J. Plast. Surg., 39: 136, 1986.
- Coenen J.M., Klasen H.J., Sau6r E.W.: Successful
homografting in an elderly patient with extensive bums using his identical twin brother as
skin donor. Bums, 16, 3: 225, 1990.
- Muir I.F., Barclay T.L., Settle J.A.: Bums and their
treatment. 3rd ed., p. 50, Butterworth, 1987.
|