| Ann. Medit. Burns Club - vol. V1 - n. 4 - December
1993
ANALYSIS OF BURNED CHILDREN TREATED IN THE BURNS
AND PLASTIC SURGERY CENTER, TRIPOLY LIBYA, IN THE YEAR 1992
Zaidi M.M., Abusetta A., Brogowski K,
Agrawal P.L., Franka M.R.
Burns and Plastic Surgery Center, Tripoli,
Libya
SUMMARY. Bum
care in developing countries remains a challenge. A prospective study of 250 bumed
children up to the age of 14 years admitted to the Bums and Plastic Surgery Center in
Tripoli was carried out during the period 1-1-92 to 31-12-92. They were categorized into
four age groups: 0-1 yr, 2-3 yr, 4-6 yr and 7-14 yr. In all age groups, scalding was the
main cause of bum. In the same period, 1924 burned children were treated in our
Out-patients Department. Admitted burned children represented about 48% of all bum
patients admitted. Epidemiological data include age, sex, seasonal variation, family size,
place of bum, time period between bum and admission to hospital, and the cause and mode of
the bum. The relationships between mortality and age, cause of bum and extent of bum are
discussed. The majority of bums occuffed in the home and in the presence of parents. Most
of the bums occurred in the winter months from November to May. Most of the patients
belonged to large families with more than three children. The male-female ratio in the age
group 0-1 yr and 2-3 yr was 1.4: 1. There were 24 deaths (mortality rate 9.6%). The aim of
this study is to implement an intense campaign to make parents aware of risk factors and
to prevent them in order to reduce the number of bum accidents.
Introduction
Bums are the most
devastating of injuries and the bum patient may suffer from their complication for the
rest of his life. In spite of recent developments in bum care, we still see high mortality
and significant morbidity in terms of bum complication and functional, social and
psychological impairment.
Bum injuries are a major problem in developing countries and indeed constitute a worldwide
problem. The incidence of bums is increasing everywhere, and consequently the incidence of
bums in childrens is also increasing.
Paediatric burns in Libya are a real problem, related to the wide use of LPG for cooking,
house electricity, the use of chemicals in the home, the use of hot water geysers in
bathrooms, large families with many children, the widespread social habit of preparing tea
at ground level, and the increased standard of living.
Children are at high risk because of their natural curiosity, their mode of reaction,
their impulsiveness and their lack of experience in the calculation of risk (Lindblad and
Jerkelson, 1990). The care of small children is dependent upon others. They cannot take
care of themselves. Bums in the home constitute the majority of bum injuries in children,
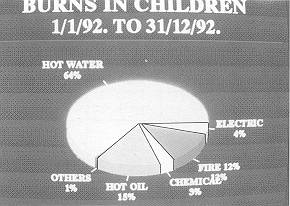
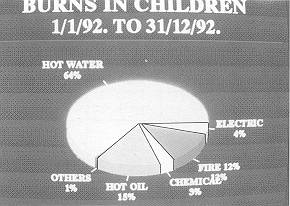
scalding being the commonest cause. Scalds constitute 64.4% of burn injuries in children,
followed by hot oil (14.8%).
Burns in children are a difficult medical and surgical problem, as children can receive
deep bums even when exposed to high-temperature liquids for just a few seconds.
The purpose of our study is to identify the epidemiological features of burn injuries
affecting children in our population which may be prevented by implementing preventive
measures and by the education of parents. No study of paediatric bums has previously been
reported from Tripoli.
Material and Methods
This article covers
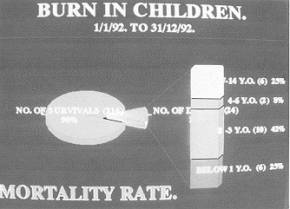
250 burned children aged 0-14 yr, divided into four groups, 0-1 yr, 2-3 yr, 4-6 yr and
7-14 yr, admitted to our Burn and Plastic Surgery Center, which is the only specialized
centre in Libya for treating burn injury victims. There are 225 beds for burns and plastic
surgery, maxillofacial and hand surgery. The bum I.C.U. has nine beds: three isolation
rooms and two big rooms with three beds each. Each room contains an air-fluidized bed, a
general bed, a bath set and Striker beds. There is one operating theatre for the I.C.U.
only and one dressing-room. All beds are equipped with proper monitoring facilities. The
ward is completely isolated, with no visitors. 'fhe personnel in the I.C.U. consists of
one chief surgeon, one chief anaesthetist, four assistant surgeons and 29 specialized
nurses. All medical care is given free of charge in Libya.
The criteria for admission to the I.C.U. are extensive burns, inhalation injury, burns
with complications and burns with other systemic problems. The paediatric bum ward
consists of two big rooms with 15 beds each and two separate rooms each with an
air-fluidized bed.
In the period 1-1-92 to 31-12-92 250 burned children were admitted to the Center. Of these
250, 41 were admitted to the I.C.U. and the rest to the Bum Department. This is shown in
Table VI.
All patients admitted, if needing resuscitation, were resuscitated according to the Evans
formula, modified for each patient according to the clinical condition at the time of
admission, patient response and age group.
The local treatment of the bum wound depended on the area involved (open or closed
method). The open method was used for face, scalp and perineurn bums and the closed method
for all other parts, with Hamazine dressing. Early bathing of bum patients is the norm in
our Center.
Further care of the bum wound depended on the depth of the bum. Superficial
partial-thickness bums were treated conservatively.
Deep partial-thickness bums were treated by early surgical intervention. Out of the 250
patients, 106 were subjected to early surgical necrectomy.
Tangential excision is our method of choice but we also perform fascial excision in deep
third-degree flame bums, the wounds being covered with skin autograft or homograft from
live donors or sheepskin graft. If the wounds are covered with homo- or sheepskin graft,
it is followed by intermingled autopatch graft every 2-3 days until all homo- or sheepskin
graft is removed.
Early nutritional support is the policy followed in our Center.
Results
A study of the
epidemiological data revealed that the incidence of bums in Libyan children is quite high,
equal to 59.24% of all patients treated in our Center. The male to female ratio is 1.4:1
in the first and second age groups and almost the same in the other age groups.
In all age groups, burns due to scalding are followed by those caused by hot oil and
flame. The causes of bum in the different age groups are shown in Table 1. Scalds were due
to hot water or hot tea. Flame burn was mostly due to gas explosion, followed by petrol
fire in older children. Almost all the accidents occurred in the home, especially in the
kitchen (96.4%).
Paediatric bums are common in the winter months, from November to May in the Mediterranean
climate. Most of the patients belonged to large families. Ninetyfive per cent of the
patients attended hospital within three hours of their injury.
One hundred and seventy-one patients (68.4%) had less than 15% BSA bums; 61 patients
(24.4%) had bums in more than 15% but less than 30% BSA; and 17 patients (6.8%) had 30-80%
burns. We did not observe bums of more than 80% in any child during this period. The
extent of injury in the different age groups is shown in Table II.
Most of the scalds were caused by the spilling of hot tea or hot water while parents were
preparing or drinking tea or when hot water was being carried. Some children were scalded
by pulling over the hot water pot. Most of the bums due to flame were caused by gas
explosion (20 patients), six patients were burned as a result of clothes catching fire and
five patients were burned by petrol flames.
In our study, the commonest burn site was the head and neck. Site distribution in the
different age groups is shown in Table III.
Morbidity and hospital stay in burned children were reduced drastically to one-half or
one-third of the days in comparison to previous years when we used only conservative
treatment in burn wounds and covered the burn wound when granulation tissue appeared.
We had no incidence of graft failure in early operated patients. We perform necrectomy
under tourniquet and we also place grafts under tourniquet. We had no cases of
post-operative bleeding making it necessary to change the dressing. Patients with small to
moderate-size bums were discharged 10 to 13 days post-burn. The hospital stay of different
percentage BSA burned children is shown in Table IV The greater the bum extent, the longer
the hospital stay.
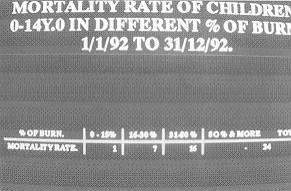
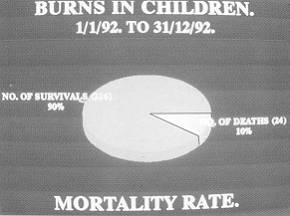
Twenty-four patients died, corresponding to 9.6% of the burned children admitted. Table V
shows mortality in different percentages and bum causes. The relationship between BSA and
bum cause shows that the deaths were commonest in flame burn patients in whom bums were
very deep, involving a large surface area, and there was associated inhalation injury.
Twenty-two of the 24 deaths followed flame burn. No patient died in the first 48 hours
post-burn. Two occurred in the home but contrasts with the findings of patients died on
day 5 post-bum and all the others died Lindblad and Jerkelson (1990). in the second to
third week post-bum. The main causes The sex ratio in this study corresponds to that of
mortality were antibiotic resistance, Pseudomonas reported by Davies (1990),
Learmonth (1979) and and septicaemia, followed by bronchopneumonia and Gorem et al.
(1988). It appears that very active and gastrointestinal haemorrhage. inquisitive boys
under five years of age are responsible Post-burn complications such as contractures,
hypertrophic scarring and keloids have decreased owing to early physiotherapy and the use
of pressure garments and neck collars, but the rate is still high. In many children
long-term follow-up is not possible.
| Causes of Bum |
Age |
0-1 yr |
2-3 yr |
4-6 yr |
7-14 yr |
Total |
% |
| Scald |
18 |
70 |
33 |
40 |
161 |
64.4% |
| Hot oil |
4 |
20 |
10 |
3 |
37 |
14.8% |
| Fire |
3 |
11 |
4 |
13 |
31 |
12.4% |
| Electric |
2 |
2 |
2 |
5 |
11 |
4.4% |
| Contact |
1 |
2 |
1 |
4 |
8 |
3.2% |
| Others |
0 |
0 |
0 |
2 |
2 |
0.8% |
| Total |
28 |
105 |
50 |
67 |
250 |
100.0% |
|
Table 1 Causes
of bums in different age groups. |
|
Percentage
Burn |
Age
Group |
0-1 yr |
2-3 yr |
4-6 yr |
7-14 yr |
Total |
% |
| 0-15 |
23 |
71 |
37 |
40 |
171 |
68.4 |
| 16-30 |
3 |
30 |
7 |
21 |
61 |
24.4 |
| 31-80 |
2 |
4 |
6 |
6 |
18 |
7.2 |
| 80 and above |
- |
- |
- |
- |
- |
-- |
| Total |
28 |
105 |
50 |
67 |
250 |
100.0 |
|
| Table II Percentage
of bum in different age groups. |
|
| Site of Burn |
0-1 yr |
2-3 yr |
4-6 yr |
7-14 yr |
Total |
% |
| Face and neck |
4 |
15 |
7 |
12 |
38 |
15.2 |
| Upper limbs |
5 |
11 |
7 |
9 |
32 |
12.8 |
| Anterior trunk |
3 |
8 |
8 |
8 |
27 |
10.8 |
| Posterior trunk |
2 |
7 |
4 |
4 |
17 |
6.8 |
| Buttocks |
4 |
18 |
1 |
2 |
25 |
10,0 |
| Lower limbs |
4 |
20 |
10 |
11 |
45 |
18.0 |
| More than one site |
3 |
16 |
7 |
11 |
37 |
14.8 |
| All sites |
3 |
10 |
6 |
10 |
29 |
11.6 |
| Total |
28 |
105 |
50 |
67 |
250 |
100.0 |
|
Table III Site
of bum distribution in different age groups. |
|
Percentage Burn |
1-10 days |
11-20 days |
20-30 days |
31-45 days |
More than 45 days, |
| 0-15 |
81 |
71 |
5 |
14 |
- |
| 16-30 |
10 |
12 |
25 |
13 |
1 |
| 31-80 |
- |
4 |
6 |
3 |
4 |
|
Table IV Period
of hospital stay in relation to percentage of bum. |
|
| Percentage of Burn |
Age |
0-1 yr |
2-3 yr |
4-6
yr |
7-14
yr |
Total |
% |
| |
Scald
|
Flame |
Scald |
Flame |
Flame |
Flame |
|
|
| 0-15% |
- |
1 |
- |
- |
|
|
1 |
0.4 |
| 16-30% |
- |
1 |
2 |
4 |
- |
- |
7 |
2.8 |
| 31-80% |
- |
4 |
- |
4 |
2 |
6 |
16 |
6.4 |
| 8 1 %
and above |
- |
- |
- |
- |
- |
- |
- |
- |
| Total |
- |
6 |
2 |
8 |
2 |
6 |
24 |
|
| % |
25 |
41.66 |
8.33 |
25 |
- |
|
|
| Table V Mortality rate in
relation to TBSA and different age group burned children in the Burn and Plastic Surgery
Center in Tripoli, Libya, from 1-1-92 to 31-12-92. |
|
Percentage of mortality of admitted children in Bums and Plastic
Surgery Center = 9.6%. |
| /Age |
0-6 yr. |
7-14 yr. |
Total |
| In Department |
156 |
53 |
209 |
| In I.C.U. |
27 |
14 |
41 |
| Total |
183 |
|
250 |
|
| Table VI Age distribution of
admitted patients in Bums and Plastic Surgery Center in Tripoli, Libya, from 1- 1 -92 to
31-12-92. |
|
| |
0-1 yr. |
2-3 yr. |
4-6 yr. |
7-14
yr. |
Total |
| In Department |
25 |
89 |
42 |
53 |
209 |
| I.C.U. |
3 |
16 |
8 |
14 |
41 |
| Total |
28 |
105 |
50 |
67 |
250 |
|
|
|
 |
 |
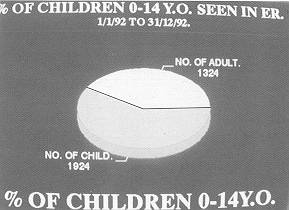
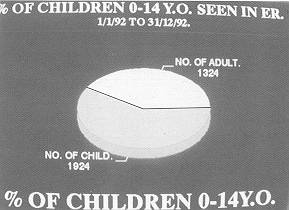
| Fig. 1 Total
number of children in relation to adults seen in Burn Emergency. |
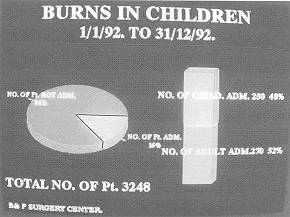
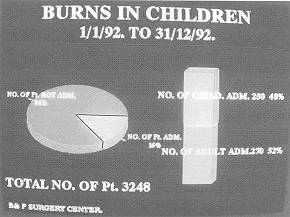
Fig. 2 Percentage
of children among patients admitted to Bum and I Plastic SurRerv Center. |
|
 |
 |
| Fig. 3 Causes of
Burn. |
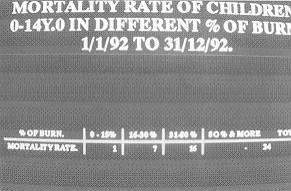
Fig. 4 Table of
mortality rate. |
|
 |
 |
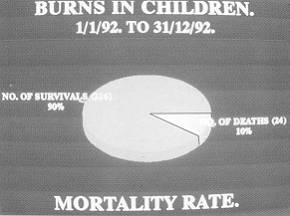
| Fig. 5 Mortality
rate. |
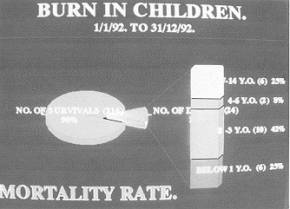
Fig. 6 Mortality
rate, age distribution. |
|
Discussion
Out of the 520
patients admitted in the period considered 250 were children, which corresponds to 48% of
all admissions and 59.24% of all patients treated in our Emergency Department. This is
consistent with other reports (Bang et al., 1992). This high bum incidence in children
forces us to investigate the causes, patterns and modes of burns in order to institute
preventive measures to reduce their frequency.
In our series, in all age groups, scalding is the main cause of bums, in contrast to
findings in other studies (Iskrant, 1967; Smith, 1969; Mackay et al., 1979), where
scalding is the main cause of bums in younger age groups and flame in older age groups.
The high incidence of scalds in children is due to their high activity, longer stay at
home and inability to protect themselves, which is consistent with other reports (Akhtor
and Gang, 198 1; Jamal et al., 1990).
Most children suffered bums in the home (96%), particularly in the kitchen (76%). This is
consistent with the findings of Davies (1990), who found that 93% of all burns in children
aged under six year for the predominant male incidence.
The general patttern of burns in relation to the various age groups is almost the same in
Libya as in western studies and in India (Muir et al., 1987; Gupta et al., 1992). Children
below one year of age are relatively immobile and receive burns from hot liquids being
spilled on them.
The overall mortality in our study was 9.6%, which is lower than that reported by
Mabogunje et a]. (1987) (13%) and Gupta et al. (1992) (19.7%) but higher than Jamal et a].
(1990) (4.3%) and Bang et a]. (1992) (3%). 'lie decrease in mortality and morbidity is not
related to a decrease in incidence but is due to recent advances in bum care.
The above study shows clearly that most burns were due to parental carelessness and
negligence. An intensive campaign to make parents aware of the dangers of floor-level tea
preparing and of allowing children to help or play around the kitchen or cooking areas and
to play with matches is necessary to minimize the incidence of bums in children. Parents
must not ask children to carry dangerous hot liquids (milk, tea or water). This study
reveals that we should provide education for parents, especially housewives, in order to
save children from devastating injuries. At present we have no organization to promote
this campaign and bum care units must therefore start the work of prevention. This will go
a long way towards reducing the incidence of bums.
RESUME. Le
traitement des brûlures dans les pays en voie de développement reste un défi. Nous
avons effectué une étude prospective sur les 250 enfants brûlés âgés jusqu'à 14 ans
hospitalisés dans le Centre des Brûlés et de Chirurgie Plastique à Tripoli entre 1
janvier 1992 et 31 décembre 1992. Les patients ont été divisés en 4 groupes selon
l'âge: 0-1 ans, 2-3 ans, 4-6 ans et 7-14 ans. Dans tous les quatre groupes
l'ébouillanternent était la cause principale des brûlures. Pendant la même période
1924 enfants brûlés ont été traités dans notre service de consultation externe. Les
enfants brûlés hospitalisés representaient environ 48% de tous les patients brûlés
hospitalisés. Les données épidémiologiques comprennent l'âge, le sexe, la variation
selon la saison, le numéro des membres de la famille, le lieu de l'accident, le délai
entre l'accident et l'hospitalisation, et la cause et la modalité de la lésion. Le
rapport entre la mortalité, l'âge, et la cause et l'étendue des brûlures est discuté.
La plupart des brûlures se sont produites dans la maison et en présence des parents, et
pendant la période novembre-mai. Le plupart des patients provenaient de familles
nombreuses avec plus de trois enfants. Le rapport mâle-femelle dans le groupe âgé 0- 1
ans et 2-3 ans était 1,4: 1. Nous avons constaté 24 décès (taux de mortalité 9,6%).
Le but de cette étude est de réaliser une campagne intensive pour sensibiliser les
parents aux facteurs de risque et pour les éviter afin de réduire le numéro des
accidents par brûlure.
BIBLIOGRAPHY
- Akhtor M., Gang RX.:
Epidemiology of bums in Benghazi, Libya. Bums, 7: 351, 1981. Learmonth A.M.: J. Ind. Med.
Assoc., 73: 43, 1979.
- Bang R.L. et al.: An analysis of
childhood bums in Kuwait.Bums, 18: 224, 1992.
- Lindblad B.E., Jerkelson C.J.:
Domestic burns among children. Burns, 16: 254, 1990.
- Davies J.W.L.: The problem of burns
in India. Burns, 16 (Supp): 54-515, 1990.
- Mabogunje O.A. et al.: Childhood
burns in Zaria, Nigeria. Bums, 13: 298, 1987.
- Gorem, et al.: Bum injury in
children. Ind. Prac.: 847, 1988.
- Mackay et al.: A comparison of age
specific burn injury rates in five Massachusetts Communities. Am. J. Public Health, 69:
1146, 1979.
- Gupta M. et al.: Pediatric burns in
Jaipur, India: an epidemiological study. Bums, 18: 63, 1992.
- Muir I.F.K. et al.: The scope of the
burns problem. In: "Bums and their management", 1-13, 3rd ed., Butterworth
Heinemann, Oxford, 1987.
- Iskrant A.P.: Statistics and
epidemiology of burns. Bull. N.Y. Acad. Med.: 43, 636, 1967.
- Jamal Y.S. et al.: Pediatric bum
injuries in the Jeddah area of Saudi Arabia. Burns, 16: 36, 1990.
- Smith E.L.: The epidemiology of
burns. The cause and . control of burns in children. Paediatrics, 44: 821, 1969.
|