| Annals of Burns and Fire Disasters - vol. IX - n. 2 - June 1996
EFFECTS OF HYPERTONIC SODIUM LACTATE DEXTRAN 70
RESUSCITATION IN SEVERELY BURNED DOGS
Ge S.D., Xhu S.H., Liu S.K., Chen Y.L.
Burn Institute, Shanghai Hospital, Shanghai,
People s Republic of China
SUMMARY. The present comparative study was
performed to evaluate the effects of resuscitation with hypertonic sodium lactate dextran
(HLD) 70 solution (HLD, Na+ 250 mmol/l, 6% dextran 70) and with lactated Ringer s (LR)
solution on the volune OfIltlid illfused, Seruill Na+ and alburnin, crystalloid
osmolarity, plasma lipid peroxide, and SOD activity. Twelve adult dogs were dividcd
randomly into two equal groups. A 35% TBSA third-degree burn was created on the back. One
hour post-burn the six animals in the HLD group received HLD (19.6 mI/kg/3 hours)
intravenously in bolus injection, followed by LR solution (6 ml/kg/% TBSA). The six
aninials in the LR group received only LR solution for resuscitation (8 ml/kg/% TBSA).
Infusion of LR solution in both groups was adjusted by maintaining urinary output at 0.5-1
ml/kg/h. The volume of fluid infused in the HLD group (5.05 ± 1.11 ml/kg/% TBSA) was much
les, than lhat ill the IR group (10.03 ± 1.30 ml/kg/% TBSA) (p<0.01). There was no
significant difference between the two group serumNa+ andalburnin, and plasma crystalloid.
Theplasmalevel of NIDA decreased after resuscitation with HI,I), which was nitich lowor
(0.81 ± 0.20 mmol/g Hb) than that in the LIZ group (1.39 ± 0.44 inmol/g Hb) four hours
post-burn (p<0.05). Plas nia Sol) activity (722) t 0.68 p/g Hb) in the HLD group was
much higher than that in the LIZ group (4.86 ± 0.53 p/g Hb) four hours pos(-bnrn
(1)<0.05), It is concill ded that HLD resuscitation could significantly reduce the
required amount of fluid infused during resuscitation coinpared with LR ,olulion,
and attenuate post-burn damage to tissue induced by lipid peroxide by elevating plasma SOD
activity. Hypertonic solutions have been reported to restore systemic haemodynamics during
resuscitation after circulatory shock more effectively and more rapidly than isotonic
solutions. , , . In particular, hypertonic saline dextran (7.5% NaCI/6% dextran 70) (HSD)
has been used as a rapid expander of intravascular volume in hypovolaemic shock` and burn
injury, , although the improvement seems to be transient and the total fluid
requirements and oedema formation remain unchanged in burns. There are however some
controversial issues in HSD resuscitation .7 The volume of fluid infused in burn shock
resuscitation varies. , In the present study, hypertonic sodium lactate dextran 70
(Na+ 250 mmol/1, 6% dextran 70) (HLD) was used in burn resuscitation. We compared the
effects of HLD and lactated Ringer s (LR) solution on the volume of fluid infused, serum
Na+ alburnin and crystalloid osmolarity. We also investigated the level of NIDA and SOD
activity in plasma 24 hours post-burn. This presented lipid peroxidation indirectly, which
plays an important role in the post-burn phase.
Material and methods
Experimental design
Twelve dogs were randomly distributed in two groups. The HLD group (N = 6) received
a 35% total body surface area (TBSA) third-degree flame burn under anaesthesia with
intravenous injection of pentobarbital sodium (30 mg/kg). One hour post-burn the animals
received FILD (19.6 mIlkg/3 hours) intravenously in bolus, followed by LR solution (6
ml/lkg/% TBSA). The LR group (N received only LR solution (8113SA). liall of llic total
amount of fluid infused was given Ill the fii,;1 eighi hours post-burn and the remainder
Ill the nexl 10 houis, Infusion of LR solution in both groups wit,,,, bv maintaining
haemodynamic stability and urillary oullm, al 05-1 ml/kg/h.
Burn injury
A 35% third-degree burn was created with intravenous injection of pentobarbital sodium
by radiation using a hroc mine tungsten lamp (5000 W) for 25 ,se(...oi)(.1,., at 75 cut
focus length. We confirmed the leslon ofilw burned skin by histological evaluation oil
itiiol),,,,y. Measurements of serum Na+ albunfin, cr , o,vllola rity and the plasma level
qfMDA alid,N 01) acin-itv Serum Na+ and alburnin were inew,,urod by nw;in,; of an ASTRA-8
biochemical autoanalysis iw,,tiunwitt (Beckman company, USA). Serun) crysl,,illoid
osinoLuNy was measured by means of an osmolmily analysis ins(in ment (Shanghai
First Medical (Inivcrsily Instiunicill Factory, Shanghai). MDA was measured occordinp, to
the TBA-fluorometic method. SOD aclivity was, measuied according to Chen et al. s
modified polaroriaphic analvscs method.
Statistical analysis
Data are presented as the mean -i- ShM lind 1,tiizilyse(f as a two-factorial
experiment willi repealed ineasures.
Comparative statistics of time effects were analysed using Dunnett s test after ANOVA by
comparing the values between time intervals with baseline values within each group.
Between groups, data at each time point were compared by using Student s impaired t test.
Statistical significance was accepted at p < 0.05.
Results
Volume offluid infused during the
first 24 hourv post-burn and urinary output
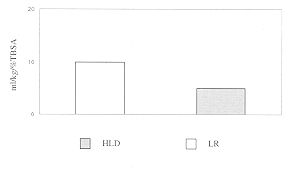
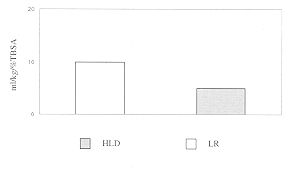
The volume of fluid infused in the HLD group (5.05
1.11 ml/kg/% TBSA) was much less than that in the LR group (10.03 ± 1.30 ml/kg/% TBSA) (p
< 0.01). There were no significant differences in urinary output between the HLD group
(0.89 ± 0.27 ml/kg/h) and the LR group (0.54 ± 0.11 ml/kg/h) (Figs. 1,2).
 |
 |
| Fig. 1 - Fluid volume infuse first
24 hours post-burn (** p<0.01) |
Fig. 2 - Urinary
output during first 24 hours post-burn |
|
Serum Na+, alburnin and crystalloid osmolarity
Serum Na+ decreased post-burn and increased after resuscitation in both groups. The
maximum serum sodium concentration was 146.2 ± 5.2 mmol/l in the HLD group and 140.8 ±
11.4 mmol/l in the LR group two hours postburn. The maximum serum crystalloid osmolarity
was 308.4 1 ± 12.8 mOsm/l in the HLD group and 300.6 ± 18.6 mOsm/1 in the LR group two
hours post-burn. Serum alburnin concentration decreased gradually after resuscitation in
both groups. No significant difference was demonstrated between the HLD group and the LR
group as regards serum sodium concentration, and serum crystalloid osmolarity (Table
1).
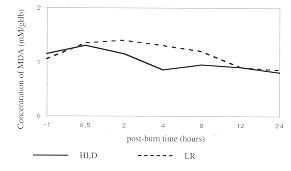
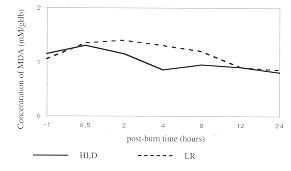
Plasma level of MDA and SOD activity
The plasma level of NIDA increased post-burn from pre-burn levels of 1.10 ± 0.45
i-niiiol/- Hb in the HLD group) and 1.07 ± 0.21 mi-nol/g Hb in LR group) to 1.25 0.38
mmol/g Hb and 1.37 ± 0.04 niniol/g Hb, respectively. The plasma level of NIDA decreased
after resuscitation. The level of MDA in the HLD oroup (0.8 1 ± 0.20 minol/g Hb) was much
lower than iiiti in the LI\ group (1J9 ± 0.44 mmol/g Hb) four hours
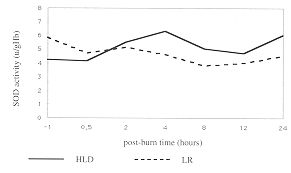
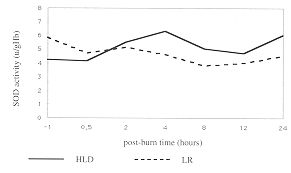
post-burn (p < 0.05) (Fig. 3). Plasma SOD activity decreased from pre-burn values of
4.27 ± 0.83 p/g Hb (HLD group) and 5.87 ± 2.24 M1g Hb (LR group) to 4.15 ± 2.72 p/g Hb
and 4.77 ± 0.83 p/g Hb, respectively, 0.5 hours post-burn. SOD activity increased after
resuscitation in both groups. SOD activity in the HLD group (7.07 ± 4.09 plg Hb) was much
higher than that in the LR group (3.89 ± 1.33 plg Hb) eight hours postburn (p < 0.05)
(Fig. 4).
 |
 |
| Fig. 3 - Changes of plasma levels
of MDA |
Fig. 4 - Changes of plasma SOD
activity during first 24 hours post-burn (* p<0.05) |
|
Discussion
Hypertonic sodium combined with dextran (HSU)), are
very c[ leenve in res ns citating animals subjected to li ici)ioj-ilia,,,ic shock, even
when given in volumes as srnall as 4 in]/kg body weight. This kind of solution
was also used in btlrll shock WSMSCi tation in animals. Although several reports
have denion strated that HSD resuscitation can improve cardiac func: tion and reduce the
volume offluid versial issues still remain. Onarlicirn Ct lf., Llsiiig an anacs
thetized sheep model of thermal injury, demonstrated that in two minutes an HSD (4 ml/kg)
bolus improved cardiovascular function compared to an equal volume of 0.9% saline
following thermal injury.
Post-burn time (hr) |
|
Pre-burn |
0.5 |
2 |
4 |
8 |
12 |
24 |
TILL)
group
Na+ (mmol/1) |
142.6 |
135.5 |
146.2 |
145.9 |
140.9 |
138.6 |
1,30. 1 |
| 10.9 |
±6.7 |
±5.2 |
±5.3 |
±13.5 |
±10.4 |
±4.6 |
| Alburnin
(mg/1) |
21.2 |
35.4 |
21.8 |
13.1 |
11.1 |
8.2 |
8.1 |
| ±12.1 |
±13.3 |
±8.1 |
+2.6 |
+4.2 |
±1.2 |
±1.0 |
Crystalloid
osmolarity (mOsni/1) |
302.2 |
288.3 |
308.4 |
310.0 |
296.4 |
284.3 |
280.3 |
| ±11.5 |
±10.8 |
+12.8 |
±8.6 |
+24.2 |
±4.6 |
±2.5 |
LR
group
Na+ (mmol/1) |
136.8 |
130.2 |
140.8 |
135.3 |
137.9 |
130.1 |
130.1 |
| ±9.7 |
±9.8 |
+11.4 |
±10.9 |
±4.7 |
±12.2 |
±10.1 |
| Alburnin
(mg/1) |
24.1 |
25.2 |
19.6 |
12.2 |
9.1 |
7.5 |
6.2 |
| ±16.3 |
±7.1 |
±8.3 |
7.2 |
±2.0 |
±1.1 |
±2.1 |
Crystalloid
osmolarity (mOsm/1) |
298.6 |
280.4 |
300.6 |
298.2 |
280.8 |
275.4 |
274.6 |
| ±11.2 |
±22.3 |
±18.6 |
±8.9 |
+10.5 |
±12.6 |
±9.2 |
|
| Table 1 - Changes of scrum Na+, alburnin and
crystalloid osmolarity during the first 24 hours post-burn |
|
The improvements were only transient.
Recent work by Tokyay et al. using a pig model of burns showed that HSD (10 ml/kg
HS13, followed by 4 ml/kg/% burn) can be beneficial in improving post-burn
microcirculation. In the present study, we did not give animals a constant LR volume, as
previously reported. After administration of an equal volume of HI-D or LR solution in the
HLD and LR groups, respectively, the infusion of LR solution was adjusted by maintaining
urinary output at 0.5-1 m]/kg/h and stable haemodynarnics in both groups. The results of
our experiment indicated that the Parkland formula is unable to maintain stable
haemodynamics in severely burned dogs, in which the volume of LR solution was twice the
amount calculated by the Parkland formula and even more. On the basis of urinary output
maintained at 05-1 ml/kg/h, our experiment showed that HI-D can reduce the volume of fluid
infusion during the first 24 hours postburn by nearly 50%, which is consistent with
reports by Schenk et al. Onarheim believes Iliat HSD resuscitation could cause
a rise of serum sodium concentration and crystalloid osmolarity. Walsh and Kramer
reported that resuscitation with dextran could increase the loss of
alburnin. Our experimental results showed (hat there was no significant difference between
the two ,roups, a s regards this parameter, which suoocsts Ilial HH) rcstiscitation does
not significantly increase dic conccnlralioil ol sodium and crystalloid osinolarity
wlicii (lit, niodk of infusion is that of our study.
There is ample evidence in the hwi;ilmc ihai oxN/pt-ii derived free radicals may be
prodticcd Atei lheiiwil injiny and that they may play an important role In 11w stibso(Iticiii
tissue damage , Although the rnechanisin undcilyinti posi iscluicmic
injury is not completely undermood mid alihou , dl oxidant-induced darnage may
ciwoinp i, s many ccil components, peroxidative deconiposihon of inombiam
lipids has been considered to I)L- Hic basis, of ccll injury.
Walsh and Kramer conl ii in(,([ di;it I IS[) i beneficial in reducing
the post-hurn rel)eifusion injury seen with LR resuscitation, while Behrinan believe that
the reduced reperfusion injury with LISD resuscitation might be the result of dextran s
oxygen free-radical scavenging and anti-neutrophil plugging properties. Our findings
indicate that HLD can decrease plasma N1DA level and increase SOD activity, which might
reduce the damage of lipid peroxidation to issue and cells.
In conclusion, HLD resuscitation cart significantly reduce the volume of fluid infused
compared with LR resuscitation. Our findings also indicate that HL,D resuscitation can be
beneficial in attenuating post-burn oxidant-induced lipid peroxidation not only by its
oxygen free-radical scavenger
RESUME. Les auteurs, dans cette étude
comparative, évaluent les effets de la réanimation avec une solution ile laciale (le
sodium dextran 70 (HLD) (HLD, Na+ 250 mmol/l, 6% dextran 70) et avec la solution de
lactate de Ringer (LR) mu le voluine du liquide infusé, le Na+ et l alburnine sérique, l
osmolarité cristalloïde, le peroxyde du ipide plasmatique et l activité SOI). Douze
chiens adultes ont été divisés au hasard en deux groupes égaux. Une brûlure de
troisième degré en 35% de la surface corporelle (SC) totale a été créée sur le dos.
Une heure après la lésion les six animaux du groupe HLD ont reçu HLD (19,6 ml/kg/3
heures) par voie intraveineuse avec injection de bol, et ensuite la solution LR (6 ml/kg/%
SC suivi par la solution LR (6 ml/kg/% SC). Lex six animaux du groupe LR ont reçu seule
ment la solution LR pour la réanimation (8 ml/kg/% SC). L infusion de la solution LR dans
tous les deux groupes a été réglée en mainte nant la production urinaire à 0,5-1
ml/kg/h. Le volume du liquide infusé dans le groupe HLD (5,05 ± 1,11 ml/kg/lY, SC)
était notamment inférieur au volume infusé dans le groupe LR (10.03 ± 1,30 ml/kg/% SC)
(p < 0,01). Les auteurs n ont pas observé aucune différence significative entre les
deux groupes pour ce qui concerne la production urinaire, le Na+ et l alburnine sérique,
et le cri stalloïde plasmatique. Le niveau plasmatique du MDA diminuait après la
réanimation avec HLD, qui était notamment inférieur (0,81 ± 0,20 mmol/g Hb) à celui
du groupe LR (1,39 ± 0,44 mmol/g Hb) quatre heures après la brûlure (p<0.05). L
activité plasmatique du SOD (7,22 ± 0,68 p1g Hb) dans le groupe HLD était largement
supérieure à celle du groupe LR (4,86 ± 0,53 p/g Hb) quatre heures après la brûlure
(p<0,05). Les auteurs concluent que la réanimation avec HLD pourrait réduire en
manière significative la quantité nécessaire du fluide infusé pendant la réanima tion
par rapport à la solution LR, et atténuer les dommages tissulaires après la brûlure
causés par le peroxyde lipidique CI) élevant l activité du SOD plasmatique.
BIBLIOGRAPHY
- Bitterman H., Triolo J., Jefer A.M.: Use of
hypertonic saline in the treatment of hemorrhagic shock. C. Shock, 21: 271, 1987.
- Gunn M.L., Hansbrough J.F., Davis JW. et a].:
Prospective, randomized trial of hypertonic sodium lactate versus lactated Ringer s
solution for burn shock resuscitation. J. Trauma, 29: 1261, 1989.
- Sondeen J.L., Gonzaludo G.A., Loveday J.A et at.:
Hypertonic salme dextran improves renal function after hemorrhagic shock in conscious
swine. Resuscitation, 20: 231, 1990.
- Hannon J.P., Wade C.E., Bossone C.A. et al.: Blood
gas and acidbase status of conscious pigs subjected to fixed-volume hemorrhage and
resuscitation with hypertonic saline dextran. C. Shock, 32: 19, 1990.
- Hannon J.P., Wade C.E., Bossone C.A. et al.: Oxygen
delivery and demand in conscious pigs subjected to fixed-volume hemorrhage and
resuscitation with 7.5% NaCl in 6% dextran. C. Shock, 29: 205, 1989.
- Horton J.W., White D.J., Baxter C.R.: Hypertonic
saline dextran resuscitation of thermal injury. Ann. Surg., 211: 301, 1990.
- Onarheim H., Missavage A.E., Kramer G.C. et a[.:
Effectiveness of hypertonic saline dextran 70 for initial fluid resuscitation of
major burns. J. Trauma, 30: 597, 1990.
- Tokyay R.T., Zerigler S.T., Kramer G.C. et al.:
Effects of hypertonic saline dextran resuscitation on oxygen delivery, oxygen consumption
and lipid peroxidation after burn injury. J. Trauma, 32: 704, 1992.
- Yagi K.: A simple fluorometric assay for
lipoperoxide in blood plasma. Bioch. Med., 15: 212, 1976.
- Chen K.M., Liao M.Y., Wna F.: The measurement of SOD
activity of plasma in severely injured iats. Acad. 1. Milit. Med. Univ., 16:23,1985.
- Maningas P.A., De Guzman L.R., Tillman FJ. et a].:
Sniall-volunic infusion of 7.5% NaCl in 6% dextran 70 tor the treatment of
severe hemorrhagic shock in swine. Ann. Ernerg. Med., 15: 113, 1986.
- Schenk W.G.: Experimental inhalation injury with
concomitant surface burn: dextran rescuscitation improves lung water and oxygenation. J.
Trauma, 30: 813, t990.
- Walsh J.C., Kramer G.C.: Resuscitation of
hypovoleinic sheep with hypertonic saline/dextran: the role of dextran. C. Shock,
34: 336, 1991.
- Till G.O., Hatberill J.R., Tourtellotte W.W. et a].:
Lipid peroxidation and acute-lung injury after thermal tratuna to skin. Evidence of a role
for the hydroxyl radical. Ain. J. Pathol., 119: 376, 1985.
- Demling R.H., Lalonde C.: Systernic lipid
peroxidation and inflammation induced by thermal injury persists into the
post-resuscitation period. J. Trauma, 30: 69, 1990.
- McCord J.M.: Oxygen-derived free radical in post
ischeinic issue injury. N. Eng]. J. Med., 312: 159, 1985.
- Behrman S.W., Fabian T.C., Kud.,, k et al.:
Microuirculnory flow after initial resuscitation of hemordinpic shock widi 7.51X,
saline/6%dexti-an 70. J. Traunia, 3 1: 581, 1991
| This paper was received on 28 March
1995. Address correspondence to: Dr
S.P. Ck., Iform Shanghai Hospital, Shanghai 200, China. |
|