Improvement of Edema and Hand Function in Superficial Second Degree Hand Burn Using Electrical Stimulation MOHAMAD T. OMAR, AHMAD M. EL-BADAWY. WAFAA H. BORHAN and ADELA. NOSSIER
ABSTRACT Objective: The purpose of this paper was to study the effect of electrical stimulation (ES) on edema reduction in seconddegree hand burn. Thirty patients with 35 hands were studied in two groups. Their age ranged from 20-28 years and percentage (9r) of the total body surface area (TBSA) w as 20 to 35. The patients were subjected to clinical evaluation at the wire of admission (history, depth and location of burn and fluid replacement) and underwent full surgical treatment (debridement and escharotomy). All patients received standard medical and physical therapy (positioning exercises and splints). The patients were randomly assigned into two groups A & B, group A: received traditional physical therapy and ES, group B: received traditional physical therapy without ES. Physical therapy evaluation was conducted 72 hours postburn in the form of measurements of hand volume, range of motion (ROM) and finger function. The serial measurement-s of the previous values were performed at the third day (post 1), at seventh day (post 11) and fifteenth day (post 111). Our patients in both groups showed that there was marked improvement of edema and subsequent hand function during the period of the study. The rate of improvement of hand edema and function were excellent particularly between the seventh and fifteenth day postburn. However, values of improvement are better in the electrically stimulated group, rather than the traditionally treated ones. INTRODUCTION The hand is vital to human function and appearance. It is also the most frequent component of burn injuries, as it is commonly used in reflex action to protect the face and extinguish the fire. The hand burn alone is not a life threatening but may seriously impair the patient's ability to function. Edema when coupled with immobilization will limit the Range of Motion (ROM). Therefore significant burn of the hand may affect physical, social, psychological and economical aspects of the patient's life. The pathophysiological changes that occur in thermal injuries include varieties of events such as loss of microvascular integrity, microvascular fluid exrtavasation, trans-capillary protein exchanges and biochemical and neurohumoral mechanism with resultant edema formation that reach steady state about I to 6 hours post-burn [2]. The amount of the fluid shift and resultant edema may be dependent on the type and depth of burn injury. Several research studies have reported that typical full and deep thickness burn gives less edema and exudation than superficial thickness burn. It also positively correlates to the exposure time [2,31]. It was suggested that edema develops when the rate of fluid is etravasated from microvessels exceeds the flow in the lymph vessels draining in the same area. The increased in the interstitial volume may be caused by increased in Capillary Filtration Coefficient (CFC), or increased net filtration pressure [4,5]. It was reported that mediators generated in response to thermal injured tissue give rise to both local and systemic effect. The increase in capillary permeability, capillary pressure and edema formation secondary to these mediators appeared to occur in two phases (1) the initial edema formation or rapid local edema formation (completed within minutes). This occurs due to release of histamine, serotonin, oxygen free radicals and Prostaglandins. (2) delayed edema formation phase secondary to increase permeability that (continued for hours). This is caused by leucotrienes, platelet activating factors (PAF) and complement fragments [2,6]. Edema begins immediately after injury and continues to increase within two to three days postburn. Therefore weakness of muscles and disturbance of joint structure can result from edema and when coupled with immobilization contributes to the formation of adhesions and disturbances in the normal sliding and gliding motion between the underlying structures. In absence of therapeutic measures, secondary changes in the articular and supporting structures will result in joint stiffness and decrease joint excursion with deterioration of function [7,81]. The role of physical therapy in management of acute hand burn should include positioning of the hand, exercises and splinting [8-111. It was believed that although the positioning and splinting prevents and reduces edema and contractures, exercises are necessary and must be integrated into the total program of therapy for burned patient in order to obtain maximum function [121]. The changes in hand edema after application of ES has been reported experimentally [131. Cathodal High Voltage Pulsed Current (HVPC) has been shown to be effective in inhibiting edema formation. While other forms of ES, such as Low Voltage Pulsed Current (LVPC), did not produce such treatment effect under similar conditions [131. It was proved that continuous and immediate application of ES has reduced hand edema significantly [151. The effect of ES on muscle strength is still controversial. Some reports suggested that ES is considered an effective means of increasing muscle strength [191]. Recently it was a common clinical practice to apply various forms of Electrical Stimulation (ES) to control acute edema; issues of treatment efficacy remain unclear. Therefore the aim of the current study was to investigate the benefit of ES in reduction of acute post-burn hand edema and improvement of hand function in superficial second degree hand burn. PATIENTS AND METHODS Between 1998 and 2001, thirty patients with seconddegree hand burn were included in the present study. They were selected from Ain Shams Burn Unit and Om ElMasryeen Hospital. The patient ages ranged from 20 to 28 years and their percentage (%) of TBSA ranged from 25 to 35, while the main cause of the burn was direct flame burn injury. The patients who had compartmental syndrome, developed infection and required grafting were excluded from the study. Only those patients who received debridement and escharotomy with local topical antibiotic and dressing were included in the study. They were classified randomly into two groups; A & B. The patients in all groups were subjected to clinical evaluation including history, location, depth and cause of burn at the time of admission. While physical therapy evaluation was performed three days after burn with edema assessment. Group A (study group); consisted of 15 patients with 17 hands. They received conservative medical, surgical and physical therapy in addition to (ES). Group B (control group); consisted of 15 patients with 18 hands. They received conservative medical. surgical and physical therapy alone (i.e. without ES).
Each measurement was repeated three times to establish an intro-racer reliability.
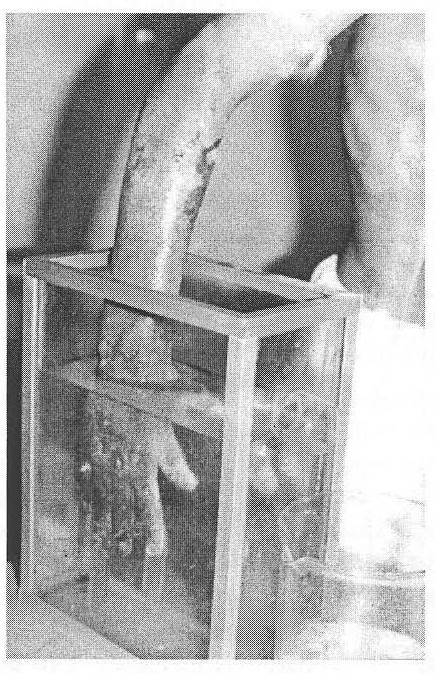
The volumeter was filled with 0.9% NaCl and allowed to stabilize until water stopped over flowing into the beaker. Then the beaker was emptied and dried and replaced under the drainage spout. The burned hand was slowly immersed in the sterilized water until the stop dowel inside the volumeter rested between the web space of middle and ring fingers. The hand and wrist remained immersed at this depth until the water stopped overflowing from drainage spout of the volumeter into the beaker. Then the beaker was moved to prevent filling during removal of the hand. The amount of the water displaced into the beaker was carefully poured into the graduated cylinder and measured to nearest milliliter. The procedure was repeated for each patient after replacing the saline and washing the volumeter to minimize risk of infection (Fig. 1).
The patients in both groups received equivalent nursing care, cleansing, debridement and escharotomy as well as traditional physiotherapy [18,19]. Physical therapy treatment included active free and active assisted ROM exercises.
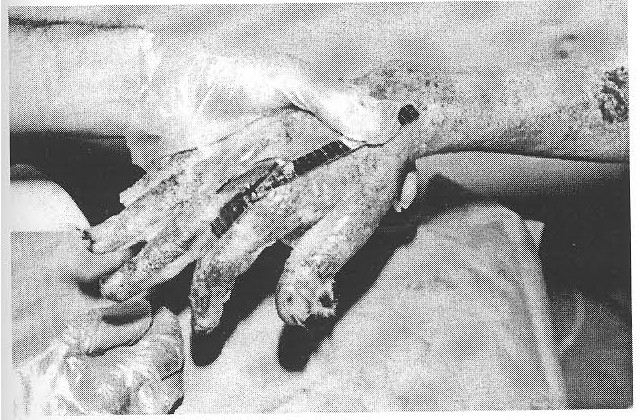
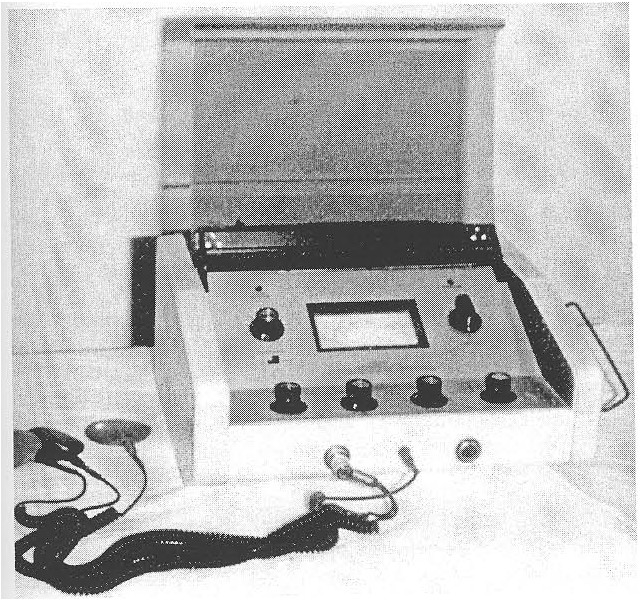
The exercises should be performed in low repitition (eight to ten times), with a two to four frequency per-day for all patients. Pushing the fingers into mass flexion to make a fist is absolutely contraindicated to maintain the balance between extensor and flexor mechanism. During treatment with ES, one active electrode (negative) was placed over the median nerve in the anticubital fossa, with the other electrode over the ulnar nerve at the medial epicondyle, after being soaked in sterile saline (0.9% NaCl). While the dispersive electrode was placed over unburned area. The frequency was set at 120 PPS with reciprocal mode of stimulation alternating between median and ulnar nerve stimulation. The intensity of stimulation was adjusted to produce minimal observable muscle contraction during 30 minutes of treatment session. The patient should not complain of any discomfort during treatment and should remain in the same position during treatment period [16] (Fig. 4). RESULTSThe results of present study showed no significant statistical difference regarding the patients ages and TBSA in edema reduction (p > 0.05).
The results of the group (A) as shown in Table (4) who received ES revealed that there were significant improvement in TAM, functional results and duration of recovery during the period of the study. There were significant increase of TAM from the beginning of treatment (Pre) value of TAM as it had poor grade of TAM for all patients and immediately after application of ES (Post I) which demonstrated good (> 180) for all patients. Also, at the seventh day, the patient exhibited excellent TAM grade when compared with pretreatment value. Finally at the fifteenth day (Post III), all patients exhibited normal TAM when compared with pretreatment value. Also, there was significant improvement when comparing the mean value at the seventh day (Post II) to that of the fifteenth day (Post IlI), which indicated continuous improvement of TAM. Functional results of this group indicated that 98%o of patients had good to excellent results and 2%n had fair results (Table 6). On the other hand 65% of patients had recorded normal use level of their fingers in less than 3 weeks after injury and 80% of patients returned to normal use level at 6 weeks post injury, while all had normal use at 12 weeks (Table 6). The results of group (B) who received no ES as shown in Table (5) revealed that there was significant improvement in TAM, functional results and time to return to work throughout the study period. There were no significant increase of TAM at the beginning of treatment (Pre) value of TAM as it had a poor grade of TAM for all patients and immediately after application of ES (Post 1). Also. at the seventh day the patients exhibited good TAM grade when compared with pretreatment value. Finally at the fifteenth day (Post III) all patients exhibited excellent TAM when compared with pretreatment values. Also, there was significant improvement when comparing the mean value at the seventh day (Post II) to that of the fifteenth day (Post III), which indicated continuous improvement of TAM. Functional results of this group indicated that 92% of patients had good to
excellent results, 6% had fair results and 2% had poor grade. On the other hand,
55%r of patients had recorded normal use level of their hand in less than 3
weeks after injury and 70% of patients returned to normal use level at 6 weeks
post-injury, while about 90% at 12 weeks (Table 6).
DISCUSSIONThe main problem in second degree burn is edema formation, which appears immediately a few hours postburn. This edema, if not properly managed may lead to fibrosis of muscles and joint structures. Thus early reduction of edema formation would prevent these complications. It was observed that all results concerning edema reduction in the first group which received ES in association with routine physical therapy had greater improvement than the results concerning edema reduction in the second group, which received physical therapy alone. The result of our study agrees with the previous experimental reports [131. However, there were no previous clinical data concerning the use of ES with edema in the hand burn. The explanation of edema reduction following ES therapy is controversial. Reduction of evans blue albumin extravasation rate early PB, was observed after application of 40 uA.DC, through silver dressing electrode. This reduction was observed wether with immediate or delayed application up to 48 hours PB), with or without continuous application. The reduction of evans blue albumin is considered as an indicator for reduction of edema formation [131. From the previous observation we can conclude that early applications of ES is an effective means for reduction of edema formation as it stimulates re-absorption and decreases accumulation of albumin in burned tissues. In the current study a protocol of 30 minutes of cathodal HVPC at 120 PPs delivered at a voltage of 10% less than VMT helps prevent edema formation and reduced hand volume immediately post-treatment and in subsequent treatment periods. This protocol was similar to that reported in previous studies and was applied to frog or rat after impact or hyper-flexion injury, these investigation revealed significant reduction of edema formation [17,18,1)1. In the present study, it was shown that the frequency of 1211 PPs at 10% less than VMT in this study was observed to be more effective than pulse frequency observed in previous studies. It was suggested that pulse frequency of 1 PPs of cathodal HVPC that induced muscle contraction, failed to significantly reduce edema formation [181; on the other hand a pulse frequency of 7 PPs was observed to reduce edema clinically but not statistically significant [161]. It was observed that cathodal HVPC used in this current study had similar effect and significant value in reducing edema formation as reported in previous studies. On the other hand anodal HVPC of 120 PPs and 10% less than VMT did not reduce edema formation. These findings suggested the importance of polarity as a critical factor in controlling edema formation via ES. It was observed that results concerning TAM improvement in group A treated via ES (HVPC) in association with routine therapy have a greater improvement than the results concerning TAM in the second group. Barillo et al., [231 used a comprehensive program of physical therapy (in the form of early elevation, splints either dynamic or static, active exercises). Their patients achieved only functional TAM at the time of discharge and normal TAM at 3 months or through an extended period of 6 to 12 months respectively. However, the results of our physical therapy regimen were better than those used by Barillo [231. All patients in ES group achieved excellent functional TAM in the seventh day post-burn. On the other hand all patients achieved normal TAM at the fifteenth day post-treatment. Previous studies have shown that early mobilization and physiotherapy in the form of active exercises in addition to splints help in reduction of edema and avoiding joint stiffness [7,11,20]. Therefore the results of group B (without ES) are going with those of Barillo et al-, [23] and Salisbury [2J]. The significant improvements that were provided in group B might be regarded to the effect of early elevation and active movement in combination with splints. The effect of limb position was investigated in early post-burn (PB) edema, as 8 hours of elevation between the 3rd and the 711, days PB was significantly effective [9]. In general, it was reported that early elevation of the distal parts of extremities is observed to be effective in the reduction of edema [23]. In our study it took 12 weeks for the patients to return to work while Helm and associates [261 found that it took 133 days and others reported that it took 99 days to return to work [24]. ES can be used prophylactically as a mean of maintaining joint ROM for patients who have a high risk of developing significant joint stiffness. Its physiological mechanism of action is not very different from the manual ROM programs. The automated and repetitive nature of the contractions however yields increased compliance when compared to a similar number of manually repeated muscle gentle stretch for antagonistic muscle group that is often considered as low repetitive stretch. ES also encourages facilitation and false improvements in the muscle that opposes the flexor group. A further potential benefit of ES is the pain relief and reduction of edema which accompanies the titanic nature of the joint motion. Conclusions: REFERENCE
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||